We've spotted something on your scan...
So a word of warning, this isn’t a blog post about web performance. I’m afraid those posts may need to be paused for the moment.
If you’ve already read the original post you can jump straight to the latest update here, or all updates here.
Note: I feel the need to point this out. This post is about a brain tumor and cancer. It’s important to realise that the doctors considerations, and ultimately treatment, are unique to my situation. Anything mentioned in this post shouldn’t be taken as gospel. If a reader finds themselves in a similar situation, please do take the advice of your own specialists. What works (or doesn’t work) for me will 100% be different for other people.
Diagnosis
To be fully upfront about all this, on Wednesday 21st April 2021 I was diagnosed with a brain tumor. Completely out of the blue. In the morning I was busy working away still trying to get Brotli compression tested and enabled on GOV.UK, 7 hours later I was given the news that I had a large brain tumor on my right frontal lobe. Hell of a day, huh!
So you may be asking: “Why are you writing about this?”. Well, there are 3 main reasons:
- I want to get this info out of my head (hah!) while I can still remember it.
- From the conversations I’ve had with people since this happened, people are fascinated with how it was discovered.
- To offer help to others in a similar situation that I (and my family) are currently in.
I’ve seemingly learned a fair amount about myself and the topic in the past 3 weeks. If you’d like to know more feel free to read on, or if you’d prefer to stick to web performance I have plenty of blog posts here which are much more light hearted!
Note: We have now enabled Brotli on GOV.UK, thanks to Jake Archibald for the humorous reminder :)
What happened?
This is a question I’ve been asked a lot. From nurses, doctors, pharmacists, out of hours doctors, and family and friends. So I’ll give you a rundown of what happened below:
Initial signs something “wasn’t right”
Back in October 2020 I started to develop issues with my lower left back and left leg. Multiple consultations with the doctors were of the opinion it was sciatica. I was given strong painkillers, told to look at getting physio, and make adjustments to my working environment. This actually all made sense at the time. Working from home for 8 months, with less physical exercise, and generally working more hours than usual, all could have easily caused this issue. Unfortunately, no matter what I tried it didn’t solve the issue. I tried: a standing desk, new office chair, new shoes, lots more walks, physio. Nothing seemed to be helping. It got so bad at one point I was crawling on my hands and knees at 3am to go to the bathroom because I was in so much pain. Not exactly what you expect to be doing at the age of 39!
After several months the back and leg pain seemed to fade, but it then turned into extreme heel pain in my left foot, which the doctor said was likely to be plantar fasciitis. Apparently runners tend to get this a lot, but I certainly wasn’t running! So yes, a fun 6 months!
But things have developed further and over the past 4 - 6 weeks I have experienced 3 seemingly very minor seizures. Throughout each I was fully conscious. I will try to describe each of them as I remember them the best I can.
Seizure 1: Standing at my desk
I now have a desk that allows me to both sit and stand very easily. I’ve got into the habit of standing for meetings with people while on a video call, but when it comes to “real work”, I always sit. This tends to give me a good balance of both sitting and standing throughout the day.
For the meeting in question I just so happened to be on mute and wasn’t speaking at the time. I suddenly felt quite dizzy and had to lean on my desk a little. At first I thought I was having some sort of panic attack. I don’t remember the topic of discussion for the meeting, but at the time it happened I was thinking “maybe this is making me anxious?”. I do remember having a really strange out-of-body experience (OBE) while it was happening. It’s hard to describe, but it’s almost like coming to the realisation that that “you are fully in control of everything you are doing” and “you have an effect on your surroundings and the people you interact with”. It feels more like a powerful emotion than anything physical. Or another way I’ve described it is imagine someone turned off the auto-pilot in your head. You are now having to consciously breathe and blink for yourself, as well as think about all the other things going on too.
Within 10 - 12 seconds this intense feeling had passed and I suddenly felt fine again. It was the first seizure I’d had, so I thought nothing of it, and simply moved on with the rest of the day.
Seizure 2: Driving in the car
This was around 2 weeks later. Now this one scares me now that I know more! Technically I wasn’t moving at the time, I was parked at traffic lights waiting for the light to turn green so I could then pull across a carriageway into the local supermarket.
Suddenly, I had the same OBE I’d felt before, where I felt like someone had pulled “me” out of the back of my own head. In front of me the lights turned green and I managed to pull forwards and start moving a little, so I had some control of my feet. Unfortunately I didn’t have the strength in my left arm to fully disengage the handbrake, so the warning alarm sounded in the car to tell me it was still engaged. I was fully conscious. My brain was telling my hand to push down and release the handbrake, but my hand simply couldn’t. It was a very strange experience where your arm and hand seemingly has a mind of its own.
Because the alarm was beeping, my wife looked over and mentioned that the handbrake wasn’t down, but she didn’t notice anything else in me that looked different. I didn’t try to speak to her, and I’m not even sure if I’d have been able too if I’d tried. Again, within 10 - 12 seconds this had all passed and I was fully able to move and control the car. We went to the shops and returned home with no further issues. Once again I put it down to a panic attack, but as it all happened so quickly I dismissed it and carried on with life. At this point I hadn’t linked the 2 separate events together.
Seizure 3: Sitting at my desk
This is the one that happened on the 21st April, the day I was diagnosed. It was around 10:50am and I was sitting at my desk working on a document. Suddenly the OBE I’d felt before came back. Only this time I lost control of both lower arms. I was unable to raise them to the keyboard to continue typing. It then developed further and I felt like I’d lost control of the lower half of my face. Almost like someone was gently pulling down on both sides of my cheeks and I was unable to stop them.
I realised this was happening, as I was fully conscious. During this time I must have tried to move, as I’d started to lean to the right side of my chair. I was rotating slowly, unable to really control my movements. Again as with the other seizures, within 10 - 12 seconds this all passed and I could again control what I was doing. But this time it was different.
With this seizure I’d been sitting at my desk, nothing strenuous was happening at all. It was quiet and I was calm. Because of this I was able to notice that I simply couldn’t control my hands and that my face had “drooped”. This immediately alerted me into thinking that I was having a mini-stroke. Now, I’ve seen the FAST campaign adverts on TV, and realised a stroke can become very serious if not acted on quickly, so that really freaked me out!
NHS 111
I immediately opened the NHS 111 website (the UK non-emergency advice service), to fill in the details of what had just happened.
Right on the front page of this service it says:
Check it’s not an emergency - Call 999 now if you have: signs of a stroke - face dropping on one side, can’t hold both arms up, difficulty speaking seizure (fit) - someone is shaking or jerking because of a fit
At this point I was thinking, “okay.. I’m going to have to phone 999” (for the first time ever in my life). But before I did I thought I’d best discuss it with my wife downstairs. I walked downstairs and calmly told her about what had just happened and also the other brief episodes I’d had weeks before (as I hadn’t mentioned them to her). We both agreed that 999 would be the best option.
It was a strange conversation with the 999 dispatcher. They were talking to me, “the patient”, asking if I was fully conscious and able to lift my arms, move my face etc. These are all standard checks for a stroke. I was able to do everything they were asking me to do with ease. At this point I felt like a total fraud, and I was simply wasting their time. I further described what had happened and that it had now passed, but I still felt a little weak in my lower arms.
I was categorised as a priority 2 (I believe) and told an ambulance would be with us within the next 5 minutes. So I quickly started to pack a few things just incase I needed to leave with them for the hospital sharpish.
Ambulance
Within 5 minutes there was an ambulance outside the door. Two very nice paramedics came in the house and questioned me about how I was feeling and what had happened. They checked my blood pressure, checked my blood oxygenation level, asked me to focus on their fingers, push & pull with my arms against theirs etc. These are all standard checks for suspected stroke patients. It turns out they couldn’t find any issues, which was embarrassing. It got me thinking: “had I just imagined this all happening?” and “am I just overacting and wasting their time?”.
One of the paramedics decided to speak to the specialist unit at the hospital to ask for advice, as they were unsure what would be best (and so was I!). After a 5-10 minute discussion I had 2 options:
- the paramedics would leave and I’d take this up with my doctor to see what was happening. This could take weeks.
- come with them in the ambulance and go to hospital for additional checks.
As I was still thinking this could be early signs of a stroke, I (thankfully!) decided that going to the hospital was the best course of action. Even if just to rule out the possibility of a stroke! So that’s what I did. I got in the back of the ambulance and 20 minutes later I arrived at the hospital and was admitted to a very busy ward.
Hospital
I’m afraid not much really happened at this point for an hour or so. I had chats with nurses and the doctors on duty, describing what had happened as I mentioned above. The doctor looking after me was a little perplexed by it all, as it was very unusual. I can’t remember the exact term he used, but I believe he was thinking these symptoms sounded like some sort of dissociative disorder. This was because of the OBE I’d described to him.
Computerized Tomography (CT) scan
As part of the standard checks I was given a CT scan. Not only that, they injected me with a special dye called ‘contrast material’. One of the side effects of this contrast is you feel like you’ve wet yourself about 20 seconds after they inject you with it. I honestly thought I’d had an accident when it happened. Apparently it’s related to the kidneys flushing the dye through your system. Either way, it feels weird!
Due to the ward being extremely busy I needed to wait for the results to be examined. This probably took around 5 hours. The first four hours seemed to go quite quickly. I had my noise cancelling headphones and a good book I was enjoying, so I was entertained (although slightly uncomfortable in the high back chairs and a face mask for COVID).
We’ve spotted something
About 5 minutes before being shown into a private room, the doctor looking after me came up to me and said the sentence:
We’ve not forgotten about you, we’ve just spotted something on your scan
Strangely enough, I couldn’t concentrate on my book or music anymore. That was a long 5 minute wait! Well, the 5 minutes passed and the doctor came back over and asked me to follow him into one of the rooms. “Fine”, I thought, “how bad could it be?”. But a few seconds later I could immediately tell something wasn’t right about his body language and manner. He seemed to be struggling to find the right words. And then he came out with it:
I’m really sorry to tell you this, but we’ve found a brain tumor on your right frontal lobe
I have to admit the rest of the conversation is mostly lost due to the enormity of what I’d just been told. It felt like the ground dropped from beneath me. But I do remember him saying it “was large”, and that “if you were to wish to have a brain tumor, this would be the type you would want to have”. A strange statement now I think about it, but one that has been confirmed since.
After about 3 or 4 minutes of chatting about who knows what, I just wanted to get out of the room. I actually felt quite sorry for the doctor. He must have done this so many times with patients over the years. I can’t imagine it ever gets any easier. I have a huge respect for anyone who has to do this on a daily basis, it must be totally crushing at times.
I quickly managed to find the words to thank him for letting me know and promptly left the room to try and work out how the hell I was going to tell my wife this over the phone. We’d been in constant communication all day via messenger, since due to the COVID restrictions she wasn’t allowed to stay with me. I knew she would be worried sick at home. It was around 7pm and she’d be getting the kids ready for bed.
I finally mustered up the courage to phone her and tell her what had been said. Again, I don’t really remember the conversation at all. But an hour or so later she’d managed to arrange childcare and she was on her way over to pick me up. She arrived and I think we were both still in shock. We didn’t really say much, other than repeating exactly what I remembered from the doctors conversation. That evening I was sent away with a concoction of drugs to start taking immediately, and then told to return to the hospital tomorrow morning 9am for an Magnetic resonance imaging (MRI) scan.
So what is it?
See, now that’s the million dollar (pound) question isn’t it. Not all tumors are the same. Some are benign, some are fast growing, slow growing, large, small etc. The CT scan could only show something was there, but not in the detail needed for a more conclusive result of exactly what.
At this point I’m going to skip ahead. I had the MRI scan the next day. Then a few days later another ‘wet yourself’ inducing CT scan. The full body CT scan was clean, showing that there were no other tumors or areas of concern in my body. Great news!
Meet my tumor
Time to cut to the chase. This is my brain tumor. There are many like it, but this one is mine. I’ve nicknamed him Gary Glia. Gary because it is a seemingly unpopular name nowadays in the UK (can’t imagine why…), so it seemed quite appropriate. And Glia because it is the type of cell in my brain that has gone tumorous.
Gary is an unpaying tenant that has taken up residence in my head. What a prick!

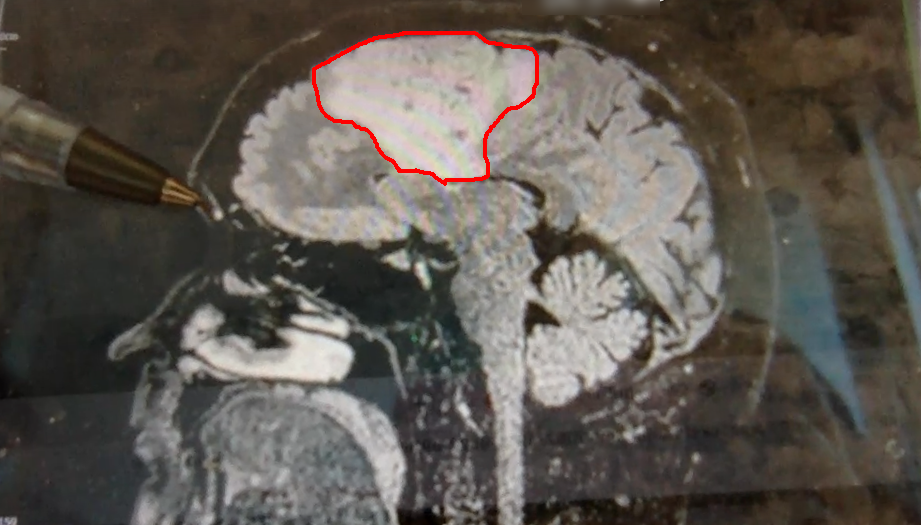
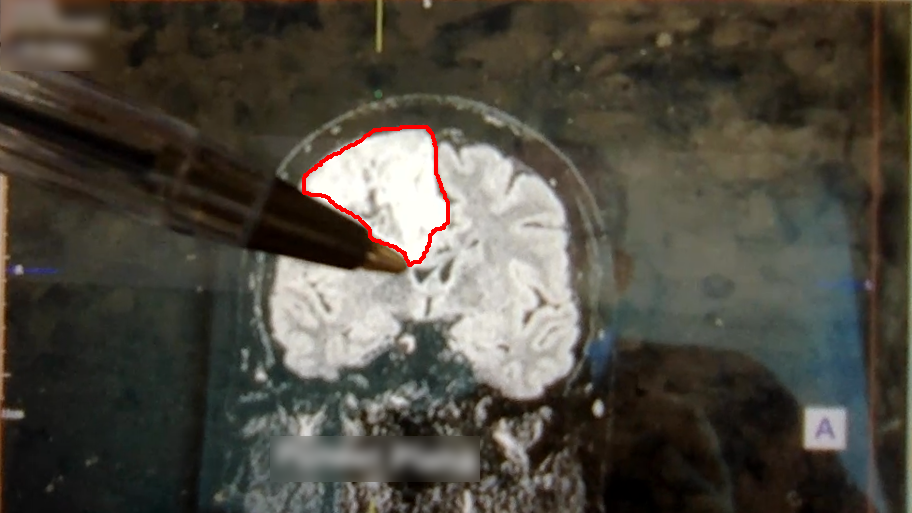
A few days later I had a meeting with the neurosurgeon where I was shown the above images. Now full respect to the neurosurgeon I spoke too, I like him. He was straight down the line and straight to the point. No sugar coating, no forewarning about the size of the tumor. After 30 minutes of chatting about all of the above, he simply pulled his phone out and showed me image number 1 you see above. You could say I wasn’t exactly prepared for the image, a understatement if ever there was one. But in all honesty I don’t think I ever would be. So it was a good tactic. Make it quick and painless, just like ripping off a band-aid!
So, what do we know about Gary?
- He’s big… look at the size of this unit. I’m amazed I can even function at all to be honest!
- He’s of the type called oligodendroglioma and currently believed to be a Grade 2 (slow growing) tumor. Wondering how you pronounce that? Isn’t YouTube great!
- He’s very rare, with only 1,217 people diagnosed with this type in the US every year out of a population of 328 million!
- He’s a number of years old. The neurosurgeon said a couple of years, but I personally suspect he could be 7 or 8 years old due to other symptoms in my past I now think could be related.
- He’s a prick.
So I’ve basically won a really shit version of the lottery… but then again maybe not. It could be so, so much worse! I actually have options that I go into in the next section. There are people out there who are given this devastating news that include words like: ‘Stage 4’, ‘aggressive’, ‘inoperable location’ and are literally given months to live, and there’s nothing that can be done. Thankfully, I’m not in that place!
The positives
I don’t want to depress everyone, so let’s focus on some of the positives I’ve since found out:
- It’s believed to be a slow growing tumor, that is currently classed as the less aggressive type (oligodendroglioma rather than anaplastic oligodendriogliomas).
- It originated and is primarily located in my brain. I have no other areas in my body showing tumors.
- It responds really well to chemotherapy. If I turn out to be 1p/19q Codeleted then chemotherapy is even better.
- My symptoms (seizures) can be managed via drugs, which now look to have minimal side effects.
What happens next?
I’ve had a really great set of meetings with some very knowledgeable folks from Oxford University and the John Radcliffe hospital in Oxford. There are three options available to me:
1 - Do nothing and active monitoring
Basically manage the symptoms and look at how the tumor progresses over time. Go for regular checkups and see how long I hold out.
2 - Biopsy to determine the exact type
At the moment Grade 2 is suspected because the CT scan hasn’t shown the usual telltale signs of Grade 3 (which is bright white ‘spots’ in the scans). Doing this would require brain surgery to remove a small portion of the tumor to be tested. I’d then need to recover from this, before a more specific treatment plan is created.
3 - Remove as much as possible via major surgery
This is the last option, and the one I’ve decided to go for. This is where the surgeon open’s my head and will try to remove as much of the tumor as safely as possible. Once completed, additional surgery may be required to remove any tumor that is left over, or radiotherapy and (or) chemotherapy can be used to finish it off.
This surgery can sometimes take up to 9 hours, and it will most likely involve me being awake for it too (so not under general anaesthetic). I find that part both fascinating and terrifying all at the same time! The reason for this is because they want to be able to ask me questions while they are operating e.g. “move your left hand”, “blink your eyes”, “speak to us”. That way, they can be sure they are minimising the damage to the good parts of my brain. It blows my mind (hah!) that it’s possible to even do this, but I’m very glad they can!
But, as with all types of surgery (especially on the brain) there are some inherent risks:
- 10-15% chance that it could cause a stroke or paralysis
- less than 5% chance of a seizure occurring during surgery. This can be very bad indeed, and will result in the operation being stopped immediately
- small chance of temporary paralysis on my left hand side
- small chance of infection due to the head being open for a number of hours
Decision
As mentioned above, looking at the size of Gary, and weighing up the risks, 3 seems like the only viable option to me that could lead to the best overall outcome. Considering I’m 39 and not in my 70’s, compared to the alternative of doing nothing, it feels like a simple decision to make. So that’s what I’m doing. I refuse to go gentle into that good night, so it’s time to make plans to evict Gary Glia from my head.
It’s also worth remembering: neurosurgeons are amazing people and they do this day in, day out, as their job! This is just a walk in the park for them…
Moving forwards
So what happens now? Well I’m now on the waiting list for the surgery, and I have additional monitoring and scans coming up. It’s basically a case of waiting for a date and managing the symptoms. If it is that the seizures come back, or anything else gets worse, then things get reassessed by the specialists and the plan changes. I’m continuing to work as much as possible, and spending time with family. For me it’s all about keeping my thoughts away from the dark places they could so very easily slip into, which I fully admit they did for the first week after diagnosis.
Support
So here’s a section I’ve compiled for readers who may find themselves in the same position as I’m now in. Thankfully, brain tumors are rare, even more so if of the type oligodendroglioma and anaplastic oligodendroglioma, so there may not be many of you out there. But if there are, here are a few support links to help you out:
- Macmillan cancer support - Oligodendroglioma
- The Brain Tumour Charity - Oligodendroglioma
- Brian Tumor Support Charity
- Brain Tumour Action Charity
- Brain Trust Charity
As you can see, there’s lots of support out there. Macmillan and the Brain Tumour Charity have been fantastic over the past few weeks. The work they do for people needs to be talked about more. They really are unsung heros working behind the scenes to make people’s lives better, in some of the most challenging times they will ever face.
Pro tip: Be very very wary of ‘Googling’ your type of tumour and reading random forums. There’s a lot of scary stats and topics out there that may be totally fictional, or only apply for that specific individuals case! A ‘random Google’ is a dangerous path to take. Trust me I did it and quickly stopped! If you can, stick with approved sources and those recommended by some of the charities listed above. Or speak to the team looking after you for advice.
Practical steps
Now, I realise there are some really terrible topics to have to talk about in the section below, but unfortunately they need to be considered. I’ve actually found the practical side of dealing with all this really useful. I’m completely powerless in terms of a future date for the surgery and the results of said surgery. But what I can do is make preparations for eventualities that may happen. It may not seem like much, but with the practical side it feels like I’m actually doing something useful. I’m moving the ball ever so slightly forwards.
So here are a few topics you could (should) start to think about:
Admin tasks
- Make sure you share passwords with your other half! I recommend setting up a family 1Password account. With a shared vault you can securely share documents, passwords, notes, all in the cloud. No need for unsecure notebooks with written passwords that could be lost or stolen!
- Cancel your driving licence and remove yourself from the car insurance. In the UK you won’t be allowed to drive if you have a brain tumor / seizures.
- Make sure your partner is listed on household bills, and can talk to the companies.
- Is your paperwork filed away in a single place and ordered logically?
- Does your partner have easy access to it all?
- Do you have a safe? If so, do they know how to get into it? Share the combination / backup key with them.
- Start to make a list of what you will need to (eventually) take to the hospital. Maybe even start to pack a bag straight away. It’s not much, but at least it’s there ready to go when needed. Involve your partner in this planning too.
Finances
- Check if your employer offers any pension scheme / death in service benefits. Is your partner listed correctly on these?
- Ensure your partner can speak / access bank accounts if required.
- Share details with your partner about your life insurance, income protection, mortgage payment protection etc. Maybe even speak to an Independent Financial Adviser (IFAs) about all this to check it is all in order.
- Are there any extra benefits you are now eligible for e.g. Personal Independence Payment (PIP)? The charities listed above can help you with advice on this.
- Consider setting up a joint account with your partner, and have shared money “just in case”.
- Create a spreadsheet with information about your household utility providers e.g. who’s your electricity provider. Include account numbers, contact numbers, cost per month, payment method etc
- On the same sheet you could include details about finances (Credit Cards, loans, higher purchases etc)
- Include details about pensions, banks, building societies you are with including account numbers and contact details.
- Remember to securely store this information (see the 1Password recommendation above)
- If in the UK you will now most likely be eligible for free prescriptions on the NHS. You can apply for this through your local doctors surgery. So make sure you do this, as you’ll likely going to need a fair few drugs over the coming months / years!
Documents
- Make sure you have a last will and testament prepared. Make sure executor’s are informed and listed correctly.
- Ensure you have your Lasting Power of Attorney in place with your partner listed, as well as backups. You can ‘do it yourself’, or speak to an specialist advisor for this. I opted for an advisor, I don’t have the mental capacity or time at the moment to do it manually.
- Make a list of questions to ask nurses / doctors etc. I’ve shared the list I made here that you can copy if you are struggling.
Above all else remember, you can make plans and be prepared, but even the most well-made plans can go pear-shaped quickly. It simply isn’t possible to pre-think and pre-plan everything for every eventuality. So there’s only so much you can do. But much that is listed above could be considered “good practice” for any adult anyway, even if you aren’t in the same situation I’m in.
Plans for this blog post
So what are the plans for this blog post? Well, I plan to keep this post updated with my progress for those who are interested. This will be the only blog post where I mention Gary the prick. Basically it will be a self-contained blog post about a topic I never expected to be living, let alone writing about! And as with my web performance blog posts, I’ll try to keep them as ‘living documents’ that are constantly updated as things change. I will continue to use the ‘Post changelog’ below in exactly the same way.
Thanks
So I have a huge number of folks to thank who have been amazing over the past few weeks:
- My wife, who has been so incredibly brave throughout this. Immediately looking for information and support that is out there (both emotional and practical). She amazes me every day.
- My parents, sister, brother-in-law and immediate both sides of the family who have rallied around to help us in whatever way they can. At the moment COVID restrictions make this hard, but this should become easier in the UK very soon. I can’t thank them enough.
- Line managers from GDS, both past and present, who have helped ease my mind when it comes to the logistics of work in the future.
- The Frontend community at GDS. I feel so lucky to be able to head up and work with such an amazing group of talented and dedicated individuals. They inspire me every day.
- A certain ex-GDS colleague who shall remain nameless. They have been a fountain of knowledge in so many different areas that, in all honesty, I didn’t even realise existed 3 weeks ago!
- And last, but certainly not least, the wonderful paramedics, doctors, nurses, and all workers of the National Health Service. The quality of care I’ve received so far has been truly outstanding. It’s all the more impressive considering the huge strain COVID is placing on the whole system at the moment. They really are heros!
And finally, thank you reader for taking the time to read the post. It wasn’t at all easy to write, but I feel so much better for actually taking the time to do it. Hopefully some of you find it useful. If helps even just a single person get through such a monumental, life changing event such as this, then it was totally worth my time writing it.
Updates
Another seizure - Monday 10th May
On Monday night I had a really ‘fuzzy’ head. That’s the best way I can describe it. It was almost like I’d taken some sort of sleeping tablet. I also had a ‘prickly’ head and scalp, quite sensitive to touch. I went to bed early but woke up at 2:30am with the same OBE I’d experienced before. I think I had another seizure in my sleep. I can’t be 100% sure as I fell to sleep again right after it. I just remember waking up to the same feeling.
On speaking to the team of specialists they said it’s most likely from lack of sleep, my body adjusting to the drugs and general stress with everything going on at the moment. They aren’t too concerned and my medication will be staying at the same level for the moment. If it gets worse in the coming weeks they will look to up the amount of anti-seizure medication.
I just need to work out what the triggers are, and the warning signs of one occurring. It’s a whole new world for me, so I don’t recognise the signs yet. You can live 39 years in a body, and still have no idea what is going on with it…
Messages of support - Thursday 13th May
I’ve been absolutely blown away by the huge number of messages of support I’ve had since writing this post. I posted it on Twitter and on LinkedIn and have received literally hundreds of messages. I’ve tried to respond to as many as I can, but I may not have seen them all. So sorry if I haven’t replied! Just to say thank you to everyone who has reached out. I really do appreciate the support. It’s all been quite overwhelming, and will admit to welling up a few times from the sheer number of them. What a crazy couple of days.
Neurosurgery pre-assessment clinic - Saturday 15th May
On the 20th May I have another appointment at the hospital. This is the pre-assessment for the surgery. I’m not 100% sure what is involved, but I’m going there with a list of questions I’m hoping to get answered. On speaking to a senior member of the team during the week the timeline for surgery has been revised down from 3 months to 4-6 weeks (assuming other higher priority cases don’t bump me down the list). This is good news, but also makes me a little anxious! I was mentally preparing myself for having 3 months to get used to the idea of awake open-head surgery. 4-6 weeks seems way too soon! But it is what it is. I’ll get used to it, it’s not like I really have much of an option…
Yet another seizure - Wednesday 19th May
A short update. I had a very short ‘mini’ seizure in the morning just after waking up, around 6:10am. I was feeling perfectly fine, then suddenly my face felt quite warm. I could feel something was about to happen. I had the feeling of losing control of my face again (drooping), then started rocking gently backwards and forwards in my seat as has happened before. I was fully aware and conscious during this time. Around 10 seconds later I was back in control. It was nowhere near as intense as some of the other seizures I’ve had, but it’s still a seizure. So it’s important to keep the specialists informed. I believe we may look into upping the dosage of the Keppra drug I am on in the coming days.
Pre-operative assessment appointment - Thursday 20th May
So today was an interesting day. I learnt a lot about the upcoming treatment and the weeks ahead. The more information I have at the better, as planning anything is virtually impossible at the moment! I had a 2.5 hour meeting with a friendly senior nurse on the team looking after me. She answered all my questions and gave me a rundown of the coming weeks, months, and years. I’ve tried to break what was said down into sections following a chronological order of future events. Ultimately the reason for the consultation was to prepare me for surgery in the future, which is a good thing. Although I’m still very nervous about the thought of a whole team poking around in my head, the information given to me today has really helped me understand it all.
Future seizures
I need to start logging any previous and future seizures, this is very important. Ultimately the plan is to achieve a sustained period where I don’t have any seizures, while keeping me on the minimal amount of drugs possible (due to drug side effects). There’s a fine balance to achieve this, and we aren’t there yet. I seem to be getting one seizure a week at the moment. I’d say my drugs will be increased in the coming days. I’ve also been asked to try to speak the next time a seizure occurs. The team has questions like: “Am I able to talk at all?”, “Does it cause slurred speech?”, “Are the words I want to say totally different to what comes out of my mouth?”. The team are interested to know how a seizure affects my speech, since this can give an insight into the parts of the brain being affected by the tumor. So that’s on my to-do list for next time!
Neuropsychology assessment
I’m scheduled to have a neuropsychology assessment in the coming weeks. I didn’t realise how important this actually was until today. It’s going to be a long process, possibly a 3 hour+ meeting where members of the team will conduct many memory and cognitive tests on me. Ultimately, this testing will be used as to set a ‘baseline’ for various aspects of my current brain function. This baseline will then be used both during and after the surgery.
It was explained to me that during surgery they will be constantly asking me questions and asking me to move parts of my body. While this is happening they will be manipulating and testing neurons in my brain to see what effect it has on my cognitive ability. Only once the surgeon is 100% happy that said part of the brain is safe to remove, will it actually be removed. As you can imagine this is going to be a long process with a tumor the size of mine! The baseline will also be used to compare brain and memory function during the recovery period. Without this baseline it would be extremely difficult, if not impossible, to measure the effect the surgery has had on me.
Only after this baseline has been established will my surgery be scheduled. That’s how important this assessment is!
Pre-surgery preparation
I’ve been given a set of items to use the night before surgery.
- Antibacterial body wash
- Antibacterial cream (for my nose to combat MRSA)
- Antibacterial mouthwash
Basically I need to be as germ free as possible before having surgery. I will be using all three of these the day before and on the morning of the surgery. Body wash all over, leave for 1 minute then rinse. Rub the cream up my nose 3 times throughout the day and in the morning. Mouthwash 3 times the day before, and again in the morning of surgery. Doesn’t sound pleasant, but if it means there’s more chance of success I’m more than happy to do it!
The surgery
Now this is where it all starts to get very interesting, as the process was explained to me in detail so that I know what to expect on the day. I will likely be told on a random Tuesday in the future that I’ve been scheduled for surgery on the following Friday. So I’ll only get 3 days notice! That’s going to be an interesting week! I’ll have a COVID test 2 days before, then on the Thursday I will go into the ward and prepare for surgery the following day.
I will have another MRI scan and a brain mapping scan. The brain mapping scan is used to map the coordinates and direction of travel which the surgeon and team will enter my skull. All this is planned to the smallest detail. Nothing like Dr. Nick off The Simpsons (thankfully!).
The surgery is likely to last 5 hours, 3 of those with me being awake. They will put me to sleep for the first hour to prepare me since it sounds a little unpleasant. I will be attached to a metal frame via a set of small screws that are drilled into my skull. I will then be woken up and won’t be able to move my head. My head will already be open. Upon waking I will be surrounded by a team of people and won’t be able to see or feel anything that is happening behind me. The team will continue to ask me questions and to do things while they operate and slowly remove the tumor (using the methodology mentioned earlier). Once they are happy, they will again put me to sleep for an hour, patch me back up and I will be sent to recovery. It all sounds so simple doesn’t it!
Recovery
Assuming the surgery goes well I will be admitted to the recovery ward for around 24 hours. I’ll have a tube coming from my head to allow fluid from the wound to drain safely away, as well as various other pipes attached to my body. The aim is to get me up and mobile (at least a little) within the first 24 hours. This is to reduce the chance of blood clots, as there’s a raised chance these can happen for up to 3 weeks after surgery. If all goes well and I don’t show signs of seizures, I will be sent home. How crazy is that, major brain surgery to home within 24 hours! If it is that there are complications, I’m unable to move etc, I will be kept in for longer. It’s all a complete unknown at the moment.
Once Gary the prick has been extracted, he will be tested to see what exactly he is (or was), and this data will be used to inform my ongoing treatment plan. Genetic marker testing (e.g for the 1p/19q Codeleted gene) will also be conducted, and this data will also be used to plan the best treatment moving forwards. The ‘default’ treatment for this type of tumor is surgery, so it’s likely I will have more head screwing fun in the future! Radiotherapy can be used once, and chemotherapy can be used multiple times to clear Gary’s leftovers should it be needed. We shall only know more after the messy uninvited squatter has been forcibly removed.
Back to ‘normal’ and work
I’m likely to need a minimum of 6-8 weeks off work. In this time I will likely exhibit changes in mood, behavior, concentration, and personality. This is all perfectly normal due to the fact that my brain will be adjusting both physically and chemically to the tumor not being there anymore. If I require further surgery and/or treatment like chemotherapy/radiotherapy, I may need a little longer to recover. Again this won’t be known until after surgery.
The key is to take this slowly. I already know this is going to be an incredibly frustrating time for me. I know myself. I’m not one for sitting around doing very little. I’m always on the go and doing something. But I’m going to have to live with it for a few months. Maybe I can start watching all of the box sets & movies I’ve always wanted to watch! Or start tackling the tonne of books I’ve never read over the years. I mean after all, it sounds better than the alternative!
A bumpy weekend - Saturday 22th - Sunday 23rd May
So it was a bit of a bumpy weekend in terms of how I’ve been feeling. I’m now on anti-seizure medication that I will be taking for the foreseeable future, maybe even forever depending on how surgery goes.
Saturday
Day went well until about 10:30am, suddenly I felt extremely tired, sat on the sofa and promptly fell to sleep. Woke up 10 mins later to find my 4 year old son had covered me in cushions and was laughing his little head off as I woke up. I was completely and utterly confused as to what had happened. The medication I’m on mentions drowsiness / tiredness, so I put it down to that. I didn’t feel 100% all day, generally quite weak. I had the same feeling around 6:30pm where I could barely lift my arms and just wanted to sleep (this is not at all like me, as I generally hardly sleep!). This feeling passed after an hour or so, after a little food.
Sunday
Went to the park with my wife and children, no issues at all. Around 1pm I had a sudden feeling of weakness. Went to the living room, sat on the sofa, promptly fell to sleep. My 4 year old son is very opportunistic, again covered me in cushions, again in hysterics when I woke up 20 mins later. He’s going to be a fun teenager…
Seizure in the kitchen - Monday 24th May
Due to everything that happened over the weekend, which we assumed were the side effects of the drugs I contacted the team of specialists looking after me early in the morning via email. I knew because of this they would be in contact with me later in the day.
Around 7:30am I was standing in the kitchen having just prepped the kids breakfast. I suddenly had what I can only describe as an emotionally driven feeling that something was about to happen. I could feel something building. I immediately recognised something wasn’t right and sat down next to my wife at the kitchen table. She could see something wasn’t right either, so stood up next to me and so as to shield me from the children. I suddenly couldn’t really control my movements and started gently rocking backwards and forwards. I was conscious and remembered that I’d been asked to speak the next time this happened. I said out loud “Can you hear me?” to my wife. It sounded perfectly clear in my head, but to my wife it sounded slightly slurred. She could still make out what I was trying to say though. Apparently while this was happening my eyes were very wide, but that could really have just been panic on my part. It all passed so quickly as they always seem to do.
Going back to the emotion I felt. I’m not sure if this was something triggered by my subconscious, as in “bubbling up” to tell me “stuff is going on here, get ready for it”, or if it was me thinking about a seizure and then this triggered it because I thought of it. I’m thinking the former to be honest.
On speaking to the specialist nurse she seemed to think that the episodes that occurred over the weekend weren’t side effects of the drugs. These were actually a different type of seizure that were happening over a longer period of time. Well at least now I know! Because of this my anti-seizure medication has been increased, and will be increased again in a week. The aim is to have a long period of time between each, or even stop them completely before surgery. So we shall see over the next week if this increase actually works.
Obtained my full scan data - Tuesday 25th May
When in one of my follow-up meetings (20th May) with a senior nurse I happened to ask the question if I could have a copy of the original photos from the scan. All I had at the time was a screenshot from a video call that was shown to me off the neurosurgeons smartphone (what a crazy sentence, isn’t modern technology amazing!). I was told to visit the hospitals radiology department, fill out a form at reception and it could all be arranged. On the form the interesting part for me was the following section:
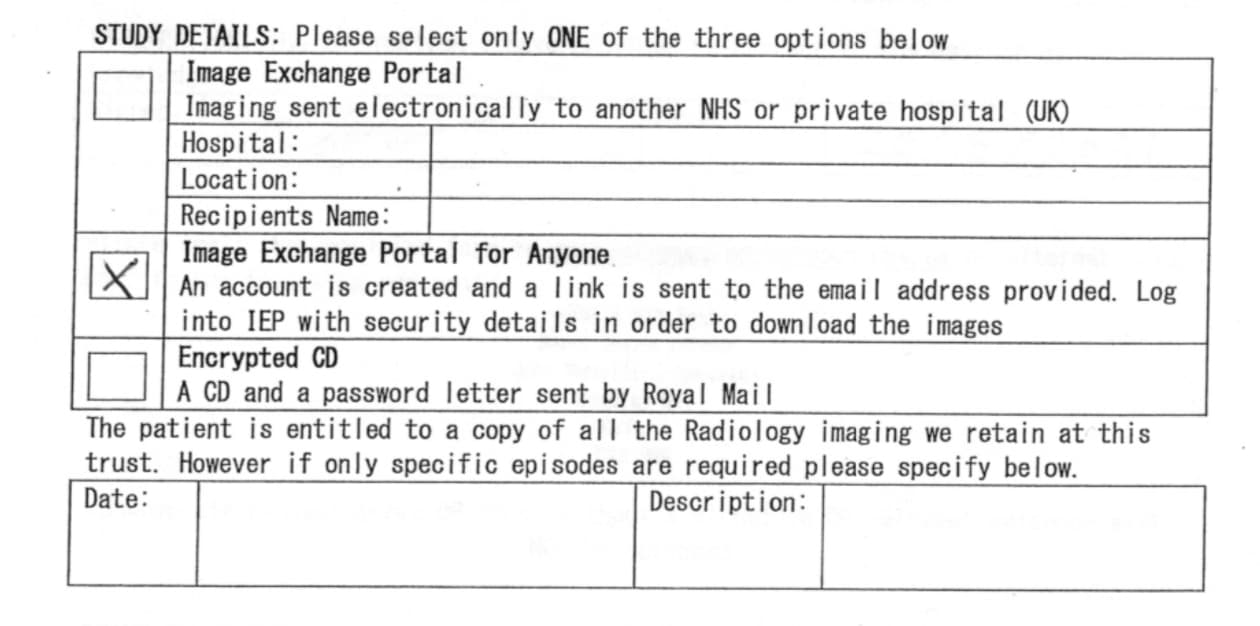
The top section allows you to choose how they send you the data. For a patient it was either as an online link or as an encrypted CD. It shows you how old the form is, no mention of USB sticks, or even DVD media! I chose the option where an online link is sent to me via email.
It’s also worth noting the sentence below this box:
The patient is entitled to a copy of all the Radiology imaging we retain at this trust. However if specific episodes are required, please specify below.
So depending on your local NHS trust, you should be able to do this yourself (should you be interested).
I received an automated email saying this could take up to 28 days, but 2 days later I had an email from a member of the team saying that my scans were scheduled for the overnight upload and I’d receive the link the following day. Upon receiving the link they sent me a one time password (OTP) via my mobile number that allowed me to login. The web performance of the system was shocking. Took around 20 seconds to load on a 50 Mbit connection and a modern browser! Thank you JavaScript…
Once I clicked on the download button I realised this wasn’t just a set of high resolution images, as it was a zip file for 1.3 GB of data! Intriguing! It took me a number of attempts to actually download the data, and I had close friends try too. Their server connection was slow and unreliable, and it also doesn’t seem to support HTTP range requests, so it wasn’t possible to resume a download after already managing to grab 880 MB of it! Best thing to do I found was to wait until later in the evening. I managed to get a download speed of around 2.7 MB per second, so it only took around 15 minutes in the end.
The reason the zip file is so huge is because it is sent in a standardized format for use in specialist tools that can interpret the data. Here’s me thinking it would be just a few images… nope! It’s literally all the images from all scans completed so far! Hence the box on the form stating which scans you require.
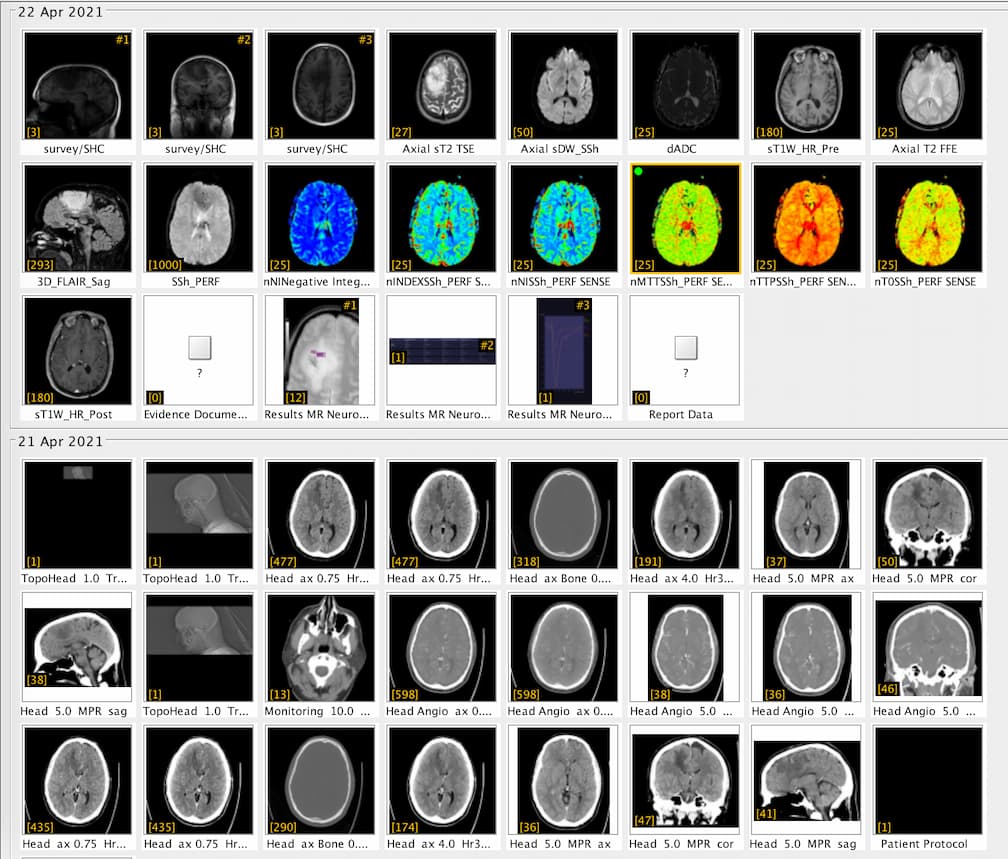
I believe there are around 4,000-5,000 images in total from 1 CT and 1 MRI scan! Thankfully there are tools that you can use to view these images. And not just view them, they allow you to navigate through all the scans. Each image is essentially a “slice” of the brain. The tools allow you to move through all 3 axis in near real time, with each of the corresponding panels changing depending on the input from the others.
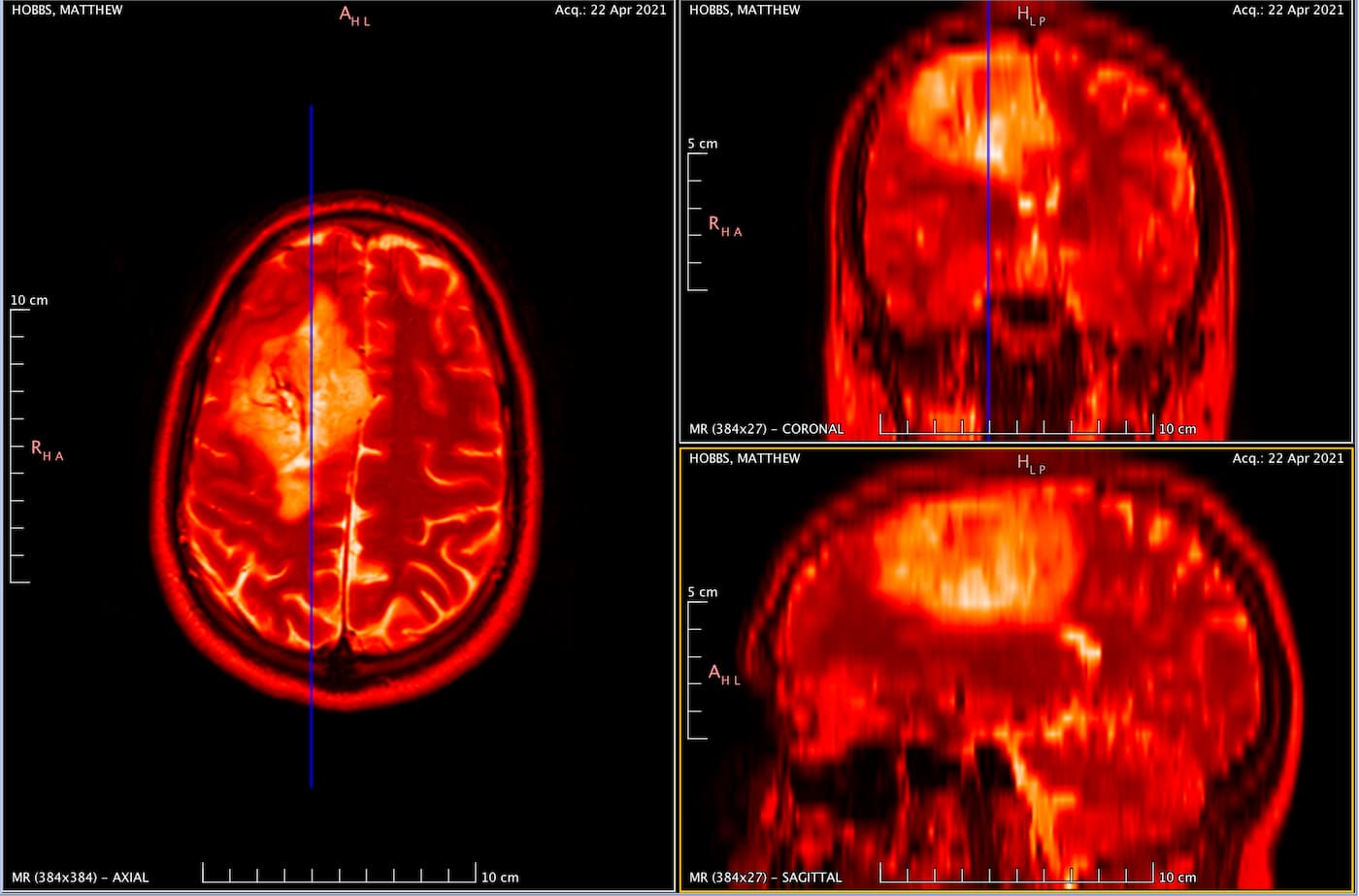
In the above image you can see my MRI scan. It’s essentially an orthogonal view of my head, with each of the panels represents a different axis:
- Left panel: Top of my head (Axial view)
- Top right: Front to back of my head (Coronal view)
- Bottom left: Side of my head (Sagittal view)
The solid blue line you see in the views is the current plane I have selected to see. As you move this plane, all three images change accordingly. Notice how the blue line on the axial view (left panel) matches that of the coronal view (top right) in terms of position. The resulting image in the sagittal view (bottom left) is the image that corresponds with this selection I have made.
It’s so incredibly clever and absolutely fascinating (to me at least)! I spent the best part of 2-3 hours looking at my own brain scans. I wish I knew what it all meant, but I plan on quizzing the experts when I get the chance. I’d like to write a blog post all about it in the future. So, watch this space!
For those interested in doing the same the tools I used are:
Horos takes it a step further, as it allows you to view your scan in 3D, and even export an animation to show all your friends at the next soirée you attend! So yes, if you ever fancy looking at your own insides in detail, remember you can request your CT and MRI scan data!
Cloudy head seizures - Friday 28th May
So I think I’ve started to recognise the signs of having a seizure. But this isn’t an obvious type of seizure that started this whole saga off 5 weeks ago. This looks to be a different type that I touched on in a previous update. In my ‘Seizure spreadsheet log’ I’ve written:
Weakness in arms, “cloudy” thinking. Feel it around my face, tingling in forehead, almost throbbing sensation. Sleepy. Hard to keep my eyes open. Muscles changing in my face (odd tightening up from the middle). Feeling coming on for a number of hours. Feels like it is building up to a seizure. Brain feels “heavy”. Went to sleep for 40 mins, felt like something ‘lifted’, may have had another seizure in my sleep. Had the same out of body experience while sleeping.
It’s hard to say, but I think I may have had another more obvious seizure while resting. I remember it happening so I did try to move my arms and they seemed fine. So who knows! Urghhh! But after my ‘sleep’ for 40 minutes or so I felt a whole lot better.
Also, I’ve noticed my left foot (heel) has started to hurt, which is one of my initial symptoms that I was blaming on sciatica. So I’m going to be mentioning that at my next catchup with the team.
Date for the memory test - Tuesday 1st June
So I’ve now been given a date for the baseline memory test. This is happening on the 29th June, a whole month away. Not ideal, and I’m a little torn with the date. In some ways I want it sooner to “get it out the way”, but in other ways I want it later. At least when it’s later it gives me more time to ‘prepare’. I still feel I have so much general life administration left to complete before the ‘big day’.
The symptoms with my left foot still persist but tend to vary day to day. Because of this I may need to be given different drugs and / or have additional scans to see what Gary is up to. I’d like to think he hasn’t gotten even bigger in the last month, but it wouldn’t surprise me!
So now I have the date. I’m guessing the operation date will be 1-2 weeks after this. So around mid-July… or in other words around the time of the F1 at Silverstone… Damn you Gary!
Back on the steroids - Thursday 3rd June
Unfortunately over the past 2-3 days the symptoms in my legs and feet have returned. I was hoping that the anti-seizure drugs were the ones keeping these at bay, but it turns out it must have been the steroids which I came off a number of weeks ago. The team have decided to put me back on a short dose so as to improve my mobility (which I’m very grateful for!). I’ll be halving the dosage in a week, then likely coming off them again the week after. Since it takes a while for them to leave your system I’m hoping that takes me up very close to a surgery date, at which point the root cause of the issue can be ejected from one’s skull!
Reduced seizures and steroid side effects - Monday 7th June
So the good news, the seizures seem to have reduced a lot over the past few days. I’ve had very little to write in my seizure log for the team. I like this direction of travel. Unfortunately as happened before the steroids have decimated my sleeping pattern. I’m currently writing this update at 00:40 and don’t feel tired at all. And yesterday I went to bed / sleep at around 3am, then woke up at 6:50am. Apparently under 4 hours of sleep a night isn’t the ideal amount you should be having! Oh well, at least I’m getting lots more stuff done!
Neurologist appointment - Thursday 10th June
Due to the seizures I’ve been having I was referred to the Neurologist who is part of the multidisciplinary team who are looking after me. It was a somewhat confusing meeting, but also very interesting that lasted around 40 minutes.
From previous conversations I’ve had with doctors, I was under the impression that the tumor was likely causing the issues I’d seen with walking in October (left back, leg, foot pain etc). But upon talking to the Neurologist and describing my symptoms, they seem to think that isn’t the case and it’s all purely coincidental. Confusing! I’d prefer it to be the tumor causing it to be honest. Having 1 major brain operation and solving 2 problems, sounds like a good deal! But alas, we shall see when Gary finally buggers off into the hospital incinerator. Only then shall we know for sure!
What was interesting for me was the conversation around classifying my seizures. I’ve been keeping a seizure log (yet another fun Google spreadsheet!). All fairly standard columns:
- Date
- Time
- What was I doing
- (Copious) Notes
Now I’d already started to notice this myself: not all my seizures are alike, and since taking the anti-seizure medication I’d started having different symptoms. The Neurologist confirmed this today. So I’ve now added another column:
- Is it a seizure involving the ‘core features’
A convoluted column title I know, but I’ll explain what It means. The ‘core features’ are effectively the most obvious (and serious symptoms). For me I’ve identified them as:
- The feeling of being ‘outside my own head’
- The emotionally driven feeling of everything being bigger than my own self (existentialism)
- Any loss of motion and control over my body
- Loss of consciousness (not happened as of yet thankfully!)
Basically if I have a seizure that displays these core features, then it is logged as one. The other seizures I’m having are still logged in detail, but not listed as a ‘core feature’ seizure.
So why is this important? Well, without this classification every little seizure suddenly contributes to what looks like an escalating number of seizures. If this is the case then getting the balance for medication is difficult. I want to be on enough to stop the ‘core feature’ seizures, but not so much that I have other side effects. This classification allows me to pull out the really important ones and therefore allow the team looking after me to see if they indeed are escalating, or if they are being managed.
So there we go, top tip if you have a brain tumor. Keep a seizure log and look for patterns in what happens when they occur!
A ‘core feature’ seizure - Friday 11th June
After the call yesterday it was all going so well. Nothing I would class as a ‘core feature’ seizure for the best part of 2 weeks. Unfortunately, one happened this evening at about 10 past 9pm. Watching the TV sitting on the floor, my wife just paused the TV to get something from the kitchen then I felt it. Again like an emotional response. Something was about to happen. I could feel it coming on. I tried to turn around and ‘shake myself’ out of it and convince myself I could stop it from happening. But within 5 seconds I’d lost control of my upper body and was shaking gently back and forth, unable to stop it.
As I’ve been told to see if my speech was affected I made sure my wife could hear me this time. She had walked in the room and not noticed what was happening so played the TV. I just started saying “Pause it”, “Pause it” “Pause it” over and over again, then eventually I said “I’m having a seizure”. Now I could have stopped myself from speaking, but I wanted to make sure we knew what the effect of it was on my speech, so I continued talking. It turns out she could hear me fine, no slurred speech. Said I sounded quite normal. I guess that’s a good thing? In total from the feeling to the end I’d guess it lasted about 30-40 seconds. Even 2 hours after it I still feel weak across the back of my shoulder blades and upper arms.
I’m hoping it was due to it being a long and busy week, maybe just tired. Or the fact that I’m now weaning myself off the steroids on the request of the Neurologist. I’m not sure! But to be honest, if I only get them once every 2 weeks, I’ll take that at the moment!
A sleepy seizure - Thursday 17th June
All has been quite quiet on the seizure front for the past few days. I’ve been gradually feeling weaker as the steroids pass through my system and my body takes over producing whatever it needs to produce… (can you tell I’m an expert in this doctor stuff!)
I’ve been getting very tired, very quickly. One moment I’m fine, 5 mins later I can hardly keep my eyes open. This happened around 5pm, just after having dinner with the kids. So I needed to go sit down in the living room. Within a few minutes I’d fallen asleep. While sleeping I’m 99% sure I had a seizure. Unfortunately due to the fact that I was asleep I’m struggling to classify it, as I’m unsure if I lost control of my arms etc, since I wasn’t moving.
The reason I believe I had one was because I remember coming too, and it felt like my brain split in two. Suddenly a pressure was released and my head felt ‘open’. I didn’t even realise I had that pressure there; it was only once it had been released I noticed the difference. I woke up a few minutes later and felt so much better, so maybe that’s how it works? The ‘pressure’ builds in my head and I don’t feel better until it is released. I’m not sure, I’m still getting used to the whole having seizures, and what triggers them.
An epiphany - Friday 18th June
It’s hard to stop yourself thinking about everything that is going on. It’s one of the reasons I enjoy continuing to work. I get to escape from thinking about the current situation and feel ‘normal’ for a short period of time. Well, at least until I remember what is happening again…
So on Friday I had an epiphany about the whole situation. I came to the realisation that I’m dying. Now I know what you’re thinking… “Damn, that got dark very quickly!” I came to the conclusion via a little thought experiment.
Imagine the wonders of modern medicine didn’t exist. No drugs, no ability to operate and remove Gary. What would be happening to me in this situation? The reason I know about any of this at all is because the tumor has got to a sufficient size to cause the seizures, so it must have crossed some tipping point recently. The tumor would be getting bigger, the number of seizures I’d be having would be ever increasing. I believe the tumor would just be getting bigger and bigger, putting more and more pressure on my brain until it eventually caused so many issues that I passed away. I’m actually on a path in my life where this would be happening to me, but thankfully I have options to try to change this path.
I like to think of all this as water slowly filling a bucket. If the bucket overflows, bad things happen. At the moment the drugs have created a hole in the bucket to help stop it overflowing, but eventually the bucket will overflow, even with the hole. The only way to stop it from overflowing is to stop the water, and that basically means removing Gary. So thank goodness for modern medicine, else there’d be overflowing buckets all over the place!
Well that was an uplifting read wasn’t it? Thanks for reading, have a great rest of the day! :)
A very good roast dinner - Sunday 20th June
Due to covid I’d not been to see my sisters new house. Not so new anymore since she moved in in February 2020! With restrictions gradually lifting and testing readily available we’d decided to go visit and have a Sunday dinner. The kids loved the adventure, investigating the house and going to visit a new park just 5 mins away.
We ate around midday. It had been a while since having roast dinner, especially since it was beef, so I may have eaten a little too much too quickly. About 5 minutes after finishing while just chatting at the table I suddenly felt incredibly tired. I simply couldn’t keep my eyes open. My arms felt heavy and I found I couldn’t concentrate on the flow of the conversation. There was no immediate seizure, but it felt like something was happening. Thankfully my sister had a spare room with a bed so I decided to go lie down to try to sleep it off.
I woke up around 1.5 hours later feeling much better. As I’ve mentioned a couple of times before, I may have had a seizure in my sleep. The ‘pressure’ in my head seemed to lift it one point while sleeping, I remember it happening. It isn’t really ‘pressure’ as such, but it’s hard to describe. Something ‘lifted’ and I suddenly felt much better.
So there you have it. My sister now has quite a claim to fame. Her roast dinners are so good they gave her brother a seizure!
The baseline memory test - Tuesday 29th June
At the beginning of the month I was told a date of the 29th of June for my memory test, so the whole month we’ve been waiting for this day. I wouldn’t say I’d been nervous. Really just anxious to get it ‘out the way’. I had no idea what was involved. All I knew was it was quite intensive and it would last a few hours. Thankfully you can’t revise for a memory test, as it did feel like being back at school waiting for an exam. The testing involved a chat with the neuropsychologist for 1 hour and then some intensive testing that lasted 2 hours.
The first part was easy. I enjoyed chatting about the situation to test myself and see what I could remember. And also to verbalise my understanding of the situation. Now I’m pretty sure the doctor had read all my medical notes, but there were points in the chat where I felt she was feigning ignorance about certain details. I’m guessing this is a tactic used to try to get me to explain my thoughts and feelings so they gather a greater understanding of my current mood and attitude to the whole situation. Not that I mind at all, it’s good to talk about all this. I often find I don’t know how I’m feeling until I try to explain it to another person.
The actual testing was really interesting. I was given around 12-14 different tests over a 2 hour period. Some were more difficult than others. There were tests that involved pronouncing words, and also remembering words. The tests always started very easy, then gradually got harder. So you’d start off thinking how smart you were, then by the end think the complete opposite! But I guess that’s the point when trying to look for a baseline result, each and every person doing the tests will find some more difficult than others.
I personally found one set of tests quite difficult. It involved thinking of as many words starting with a particular letter in 60 seconds. The only rules were they couldn’t be a person’s name or places. Any other word in the english language starting with that letter. There are that many surely it can’t be that hard! Well apparently not. For some reason my brain was insistent on thinking of swear words starting with whatever letter I was given. So each and every time I’d think to myself, “No I can’t say that word, it’s rude…”. Once you get into that little game with your brain (“say that, it would be funny!”), It’s hard to stop! Thanks brain! I think I could only think of between 10-15 words in 60 seconds. Not many at all so I’d say I’m below average for that test!
The easiest tests I found were the ones involving patterns. Look at this sequence of colours and shapes then pick the next one in the sequence from a list. I think I did okay in those tests, but who knows! Maybe I’m below average for those too.
The testing was intentionally hard as this is to try to gauge where you’re at and set that baseline. After surgery they can then repeat the test and look at the difference between the two sets of results. I guess since there were lots of different types of tests, if they see a drop in the results for one type of test, it suggests a change in a certain area of the brain. It’s all very clever!
Now with this date out the way, it’s just waiting on a date for surgery. All I know is that it is likely to be at some point in July. So July is going to be an interesting month!
Shielding - Sunday 4th July
Unfortunately there’s been a number of positive covid cases at my children’s school. Year 2 and year 5 have been isolating at home for 10 days. We’ve been testing every day, and have been for a drive-through PCR test. Thankfully they all came back negative!
With both children back at school, and covid literally so close (there are a number of schools in Oxfordshire having similar issues), my wife and I decided that it would be best if I were to shield. It’s pretty crappy to have to avoid your own children, but having waited 2.5 months for a surgery date I really don’t want to lose it because I catch covid. That would be bad!
So I’m now staying with my parents. It’s the first time I’ve lived with them in 21 years! I’m still working and plan to do so, up until I get a surgery date. This will happen on a Tuesday at some point in July. Every Tuesday they triage the patient list and make plans for the week. So I’ll receive a phone call saying surgery will be on Friday! You don’t get much notice, only a couple of days. Although that’s probably a good thing. I don’t want to be dwelling on the fact that they are going to be removing part of my brain in a couple of days for too long!
When folks have asked me how I’m feeling about it all, It’s hard to describe. In some ways I want the surgery to happen right away to at least “get it out the way”. But in others I don’t want it to happen at all, as it really is a watershed moment in my life. There’s always going to be a ‘pre-surgery’ and ‘post-surgery’ me from beyond that point. Fingers crossed those two versions of me don’t change much!
I’m siding on the fact that I actually want it done now. My family and I have been in limbo for a few months now, so it would be good to be able to move forwards and start to actually plan things! I’ve gained so much respect for people who are on transplant lists for years. Waiting for hearts, kidneys, livers etc. I’ve only been waiting 2.5 months and it has felt like an eternity! I can’t even imagine living your life waiting years for surgery. Not being able to properly plan anything because “what if we get the call?”.
My next update will likely be when I have an actual surgery date. Not too long I hope!
No news - Tuesday 6th July
So having waited around all day for a call from the hospital, it unfortunately never came, so no surgery this week. Annoying but at least it gives me a little more time to get a few more things done! Let’s see what next Tuesday brings!
In other news, there’s been a few more reports of covid in schools in Oxfordshire so I still feel sheilding was the right thing to do!
Still no news - Tuesday 13th July
Mid-way through July now and still no news about surgery. I was hoping to have it at the start of the month so I could at least start the recovery process and maybe have the latter end of the summer to do something “normal”, (whatever that means in 2021!).
Being on the waiting list for hospital appointments is pretty stressful at the moment as covid cases are surging, I really feel for the folks working in the NHS at the moment. It must feel like a never-ending tsunami of stress and unpredictability.
Well at least I’ve been given a date of “July”, that’s a lot more than some people have! I’ve a sneaking feeling it will be right at the end. Fingers crossed the next few weeks go quickly. Although, saying that, these past few months have been the longest of my life!
Between Life and Death - Thursday 15th July
Earlier in the week I discovered there’d been a short series on Channel 4 here in the UK called “Brain Surgeons: Between Life and Death”. Reading the synopsis it all sounds very interesting. I thought it would give me some insight into what to expect on the day. Unfortunately I wasn’t mentally prepared to watch it. I made about 5 mins into the program and had to stop. It hadn’t even got to any of the surgery yet and was just talking about the people and their families. I think that brought it all home how serious this all is, not just for me but for everyone around me. What finished me off was seeing the guy lie down on the operating table and realising in only a few weeks time I’m going to be doing exactly the same. It’s not a pleasant position to be in.
I mean let’s be honest here, the clue is in the title: “Between Life and Death”. It probably isn’t the best thing to be watching weeks before major brain surgery! Saying that, I do plan on watching it post-surgery. I’ll have a very unique perspective of what it’s like from ‘inside’ the process. I can then compare notes from ‘outside’ the process too.
Close but no brain surgery - Friday 23rd July
So this week has been quite a rollercoaster. For the past 3 weeks I’ve been mentally preparing for a date of the 30th July for surgery. Now, I realise none of this is set in stone, but as that’s the only date you’re given it tends to be the one you focus on. Unfortunately I had an update at the start of the week stating that the date was going to have to be pushed back. It sounds like I was actually quite close, but a few emergency cases came in that took priority. So I’m back to the 2 week holding pattern (which really sucks!).
Saying that, I was given some interesting information during the conversations I’ve had with the team. Another MRI scan has been requested as I’m coming up to the 3 month point since diagnosis. But this isn’t your usual MRI scan. It’s actually being pitched as the pre-surgery scan. The neurosurgeon (and team) would like to understand what Gary has been upto over the past 3 months. From what I understand, this will be a more detailed scan that can be used for surgery planning. I don’t know if this means it will take longer, or if they just conduct more scans / more detailed analysis(?) I guess a question for the test operator when I meet them soon.
I was also given information that the operation is likely going to take longer than expected. The team usually conducts 2 operations on the Friday of each week. But the neurosurgeon is now considering only operating on me on the day, due to the size of Gary. I’ve yet to decide if this is a good or bad thing? Good in the fact that they can take their time to extract “the prick”, but bad in the fact that it is needed (and I’ll be awake for most of it!).
Fingers crossed the 6th August materialises. Folks have said to me that the waiting is the worst part. I’ve no way of knowing that at the moment, but I’m happy to agree. It is pretty bad! Let’s see what next week brings I guess!
Pre-surgery MRI scan - Monday 26th July
Today I had my pre-surgery MRI scan. Now that suggests that I have a date for surgery, but alas no, not yet. I’m supposed to have an updated scan every 3 months to look at what Gary has been up to, so instead of having 2 scans in a short period of time, the standard scan has been upgraded to a pre-surgery scan. This means that the scan takes a little longer than usual (around 40 mins). They take more detailed scans and I assume maybe a few more types? This means there’s no ‘blocker’ for surgery now. When I get a slot, I’m not waiting on an MRI scan. This is good news!
The scan itself was fairly easy. There was a slight miscommunication so I was waiting around 30 mins longer than needed, but compared to how long I’ve been waiting for surgery it’s nothing. At least it is done! 40 minutes stuck in a cold, confined tube that screams at you like a ZX Spectrum isn’t the most relaxing experience. At 35 mins in they came in and injected the contrast into my arm via the cannula (I hate cannulas, so uncomfortable!). It was cold as it ran up my arm. A few seconds later I could swear I had a mini-seizure. I had the ‘emotional’ response I’m getting used to, but since my head was tightly strapped to the MRI table and I was lying down in a confined tube, I’m not sure if it affected my movement. I’m going to raise this with the next doctor I speak to. Maybe it’s a known side effect?
As another Tuesday rolls around, here’s hoping I get any news on a date for surgery. The wait is really starting to get me down.
One confusing week! - Sunday 1st August
The last week has all been a little crazy. On Monday I had my 3 month MRI scan, which was also the pre-surgery MRI scan too. I’ve mostly been on annual leave from work as there’s just so much going on it’s hard to concentrate on anything else.
On Tuesday I was back to work for the day, but something unusual happened. I was in a meeting with my incredibly supportive line manager, but 30 mins into our 45 minute video call I had to stop quite abruptly. I completely lost my train of thought and felt like I was on the cusp of having a seizure. Thankfully I can now recognise the telltale signs of this happening. This is a worrying sign as work has been a haven for me over the past 3 months. I’ve been able to zone out of “real life” for a few hours and concentrate on work, completely oblivious to the fact that Gary even exists. For a few hours at least! It now seems that even this little haven is eroding.
On Wednesday I had a call from the hospital with the results of my Monday scan. It’s a bit of a mixed bag. The good news is that the tumor hasn’t grown in the past 3 months. The less good news is that there’s still no date for surgery. The bad news is that some swelling can be seen around the tumor, also known as cerebral edema. I think this explains the symptoms I saw on Tuesday.
Thursday and Friday were a bit of a writeoff to be honest. All day I wasn’t feeling 100%. Incredibly sleepy, dizzy and at times quite confused. It’s strange, and it comes on so quickly. One minute you feel fine, next minute it all changes for no apparent reason. Thursday evening was particularly bad, where I could barely keep my eyes open or even really speak to my wife. I was completely disconnected from reality and didn’t have the energy to even try to re-engage.
On Friday evening it got so bad that my wife decided to ask for advice from the 111 team (non-medical emergency number). We went through the triage process and eventually the very nice on-call GP was sent out to see me. She was satisfied I didn’t need to go to hospital but did want to phone the specialists in the oncology and neurology departments. On speaking to the on-call neurology consultant who looked at my scans they recommended that I should be back on steroids to reduce the swelling in my brain.
Now here’s the difficult part. The team I’ve been under the care of for the past 3 months have been very keen to take me off steroids when I’ve been on them, since they are quite strong and have some nasty side effects. Steroids take around 2 weeks to leave your system once you take them. So I’ve been stuck between a rock and a hard place. Take the steroids and I could potentially compromise a future surgery date. Don’t take them and my symptoms could get worse.
Weighing up these options, it was 100% my decision NOT to take the steroids until I’ve been given the all-clear from the team looking after me at the hospital. There’s no way I want to lose the opportunity of surgery because I took a drug that is now in my system for weeks. So due to the fact that I was having unpredictable symptoms from the swelling, I’ve moved back with my parents for a few days. At least they can easily keep an eye on me without having to keep two young children entertained.
So there you have it, quite an eventful week! I’m seriously hoping that the upcoming week is the one where I’m given a surgery date. I don’t think I can cope with much more waiting around “treading water”. Roll on Tuesday. Fingers crossed the phone call!
The brain fog has lifted! - Friday 6th August
Yet another crazy week with quite a few highs and lows. I’ve been using some of my annual leave to get a few things sorted before the surgery. If I’m honest, I haven’t managed to do much for the past few weeks which is very frustrating. Being so tired and dizzy makes it hard to concentrate. I’ve been sleeping a lot and very rarely left the house.
Tuesday came and went with no real updates about a surgery date which was very disappointing. I did hear back from the team at the hospital about the steroids, so from Wednesday morning I started on them again (to reduce the swelling around the tumour). Wednesday and Thursday there was some improvement like they were beginning to make a difference. I had much more energy and I could finally walk properly again (as the issue with my foot has returned).
But it was today (Friday) where I’ve really felt better. The best I have felt in weeks to be honest. I realised while having a shower this morning that I was actually thinking and planning out my whole day ahead of time. Multiple streams of thoughts about everything I wanted to get done. I’d not had this ability for a few weeks. It has literally been quite ‘single threaded’ (there’s a web developer term for you). Basically I’ve only been able to focus on the single task at hand, nothing more. I must admit I didn’t notice this change, it was only once I ‘reverted back’ to feeling normal again I realised it had happened. So yes, I went into overdrive with work today because I could finally do things again! I worked until 7:30pm (naughty I know) getting tonnes of stuff sorted, and started making plans for the department’s stance on legacy browsers (cough… IE11), which should come into effect in March to June in 2022. So planning almost 10 months ahead of time. I simply couldn’t have done that even 3 days ago.
Next week is going to be interesting. I have a couple of meetings with the hospital to go over symptoms and then speak to the neurosurgeon again. I have lots more questions for the team. So let’s see what next week brings! Maybe some clarity on a date, like I’ve had from the steroids over the past few days. That would be nice!
Another mixed few days - Sunday 8th August
Well it has been an odd weekend symptoms wise. Friday was a very good day. The best one I’d had in a while actually. I could finally think clearly again. Unfortunately I think I went a little bit overboard!
Saturday
I really paid the price on Saturday. As Friday had gone so well, we decided to head out to an open day event for a charity. We were under the impression it wouldn’t be particularly busy, but unfortunately not. It seemed like everyone had turned up. This isn’t a bad thing in terms of covid as it was all outdoors and we all kept our distance. It was just the sheer number of people, sounds, noise, interactions… the general busyness of it all that broke my brain.
I lasted about an hour then had to admit defeat and go back to the car to sleep with some quiet music on for 2 hours. I believe this was a mixture of the tumour, swelling, and having just started taking steroids. Apparently steroids can heighten your senses, making sounds louder, colours brighter etc. I think it was a combination of it all that my brain just needed to get out of the situation.
Thankfully after a couple of hours of rest and getting home I felt much better, and ended up doing virtually very little for the rest of the day.
Sunday
After a great Friday and poor Saturday we decided that I best not risk doing much, so I mainly pottered around the house looking for little bits to keep me occupied. I’ve certainly noticed that I’m much more comfortable and settled while at home. I’d assumed it was all a part of the past 18 months and the pandemic, but I’m beginning to think it is all interrelated. I think (unknowingly) to me this tumour has been developing and growing and it has been changing how my brain works and thinks. Although I don’t feel anxious about leaving home, there’s always something in the back of my head where I can only fully relax once I’m back.
Now, day to day you don’t notice this, why would you after all? Such small changes. It’s just like watching your children (or pets) grow up. Day to day you see no change, but looking back everything has changed. So when these subtle differences are compounded over months (and even years), then you see the huge change staring you in the face. The more I think about it, the more it makes sense. My brain is actively looking for a place with the least cognitive load. Familiar surroundings and people with complete predictability. This equates to a brain that doesn’t need to do much (which is good when you have a brain tumour!).
Annoyingly on the flip side, the steroids seem to give me enough energy to put me on edge (almost twitchy), but then I don’t have the energy or brain capacity to do anything particularly useful with it. Stuck between a rock and a hard place really. So the day was mainly resting and mentally preparing myself for another week of uncertainty.
The week that will never end! - Wednesday 11th August
Well, the title says it all really. This feels like it has been a very long week. I’ve had 2 important meetings at the start of the week, and after those it’s hard to believe there are still more days left to go!
Monday
Since starting back on the steroids last week to reduce the swelling on my brain the team has wanted to keep a close eye on me. If there’s one takeaway from the past 3 months it’s that they don’t want me on them! That’s fine with me, I’m happy to listen to the experts!
So I had a general catchup with the nursing team going over my symptoms since I started back on them again. I explained the highs and lows of the weekend and it all sounds like classic steroid side effects. One day you feel on the top of the world, the next day you are back in the depths. When you couple it together with the tumour, swelling, and the fact that steroids obliterate my sleeping pattern (3-4 hours a night when on them), it all makes sense really. I’m on mild sleeping tablets to combat the issue, but they don’t work too well.
The rest of the call was mainly to prepare me for the Tuesday call with the neurosurgeon. I’d already started making a list of questions, but off the back of the conversation I now had a few more. The more information you can get from the person who will actually be operating on you the better really!
Tuesday
I worked in the morning as the call wasn’t until the afternoon. For some reason I was very nervous about the whole thing, so I was glad to have the distraction. I’m not quite sure why I was so nervous, but it’s always in the back of my head: “maybe they made a mistake, and the 2nd scan will show a much worse prognosis”. Unlikely I know, as I’m sure they would have mentioned it, but it’s hard to stop thinking about it!
But overall the 45 minute conversation went really well! There’s been no growth in the tumour size over the past 3 months which is amazing news. The tumour still looks to be of the type oligodendroglioma. The fact it hasn’t grown point towards it still being grade II and not anaplastic oligodendriogliomas (grade III). We still won’t know this for sure until 10 days after surgery, as that’s how long it takes to get biopsy results back.
The swelling around the tumour isn’t as bad as thought. Only slight swelling really. But this then points to the fact that the symptoms I’ve been getting (dizziness, ‘fuzzy head’, loss of concentration, disconnection with the world etc) all relate to the tumour itself. I’m not sure which I prefer it to be, the tumour or the swelling!
I got to ask lots of great questions and get most of the answers I needed. One of the fundamental takeaways is that I “must not get covid”, (direct quote from the neurosurgeon). I’m more than happy to keep to that! Having been double jabbed and not really going out, I’d hope the chance is pretty slim anyway.
The main discussion was around a date for surgery, and this came up almost right away. The team were very apologetic that it had taken so long, but the pressures on the whole system at the moment are large. Now as I seem to have a grade II tumour that is large (but not aggressive) this drops me down the priority list somewhat. There are some types of brain tumour like the glioblastoma that are really really aggressive and can’t be cured. The neurosurgeon explained that in these cases sometimes you only have a matter of days / weeks where you can make any difference to a patient’s life expectancy! So at the moment I’m now top of the list, barring any emergency cases coming in. So in theory I should hopefully be operated on in the next two weeks(!). Off the back of the meeting we are looking at a date of “August”. If this is the case, it fits well with the children going back to school in September, as I can see the risk of getting covid in this period increasing once they are back. And what with my instructions “not to get covid”, these two worlds don’t fit together!
I asked about how big he thought my tumour was. I’ve already exported a 3D animation of Gary which you can see here, but I wasn’t sure actually how big ‘he’ is in terms of numbers. The neurosurgeon estimates that ‘he’ is taking up around 10-15% of my brain. That’s pretty impressive! So I only have the capacity to use 85-90% of my brain anyway. I also asked the question if this is the type of tumour I could have had since birth, and I’ve just grown up with it? The answer to that was a blunt “no”, so that’s the end of that conversation then!
I found out a more about the operation itself and recovery period:
Operation
It is likely to take 6-9 hours, with me being awake for approximately 6 of those hours. That sounds like a hell of a long time to me, but the neurosurgeon assures me it will go quickly. He said I’d be surprised how quickly it passes, so watch this space. I’ll let you know after the event! A successful operation is where he manages to remove around 80% of the tumour, leaving the rest to be removed via other means (radiotherapy / chemotherapy / additional surgery).
Recovery
Now because the tumour is so large and deep into my brain, it comes with a few risks (as I’ve mentioned before in the original post). One of the main risks is the fact that the tumour is wrapped around my motor cortex, which is the part of the brain that controls limb movement. As Gary is sitting in my right frontal lobe, any issues will occur on my left hand side (since the brain is reversed in this respect).
The neurosurgeon explained that there is something like a ‘switch’ that can effectively turn on and off if the brain is damaged (or changed). During the operation there’s no warning that this will occur. One moment I could have full control over my left arm / hand, the next moment nothing. Quite a scary thought really! Thankfully in most cases this is only temporary and lasts 10-14 days. It’s very rare that it is permanent. Over time, as the brain re-adjusts to being without the tumour, it relearns how to process limb movement and the ‘switch’ is turned back on. If this were to happen, my seemingly ridiculously short 24-48 hour stay in hospital will turn into a couple of weeks in rehabilitation. So there’s just another unknown to throw into the mix!
So that was mainly what I learned from the first two days of the week! Quite a lot to take in, and there are still 3 days left to go! I plan to take it a little easy to process it all and start mentally preparing myself for the next two weeks, where there’s a lot that can happen very quickly indeed. I feel I’m about to reach a watershed moment in my life. There’s forever going to be a pre-surgery me, and post-surgery me on the horizon.
Tune back in soon for more on the eviction of Gary ‘the prick’ Glia!
Houston, we have a date! - Tuesday 17th August
So it’s been over three months since I was first diagnosed, and I must admit I’ve no idea where the time has gone! In some ways it feels like it has gone quickly, but in others it feels like it has been the longest three months of my life! Living your life in weekly chunks isn’t much fun. Waiting for every Tuesday to come around for a surgery date is quite stressful. The day comes and goes with a whole range of emotions. A mixture of anxiety, excitement, all the way through to disappointment and sadness, then rinse and repeat for another week.
Thankfully the waiting now seems to be coming to an end as I’ve finally been given a date for the operation: Friday 27th August, or G-Day as I’m calling it. G-Day stands for “Gary get the f*ck out of my head”-Day. The plan is for me to go into hospital the day before and stay overnight, with the operation happening on the Friday morning. It should last approximately 8-9 hours. Beyond that is a big unknown, so we’ll have to see how it goes!
Unfortunately, there is always a chance that it could be cancelled at the last minute, or the hospital doesn’t have a bed for me. If this happens there are multiple options. The nurse explained: “Plan A is the aim, but plans B-E also exist too”. We will only know the plan I’m sticking to on Thursday. It will be a relief to get a hospital bed, as that’s the final step before surgery!
In other news: I also found out that during recovery I’m going to need to wear deep vein thrombosis (DVT) stockings for 1 month(!) after surgery. Night and day, 24/7! Apparently the risk of blood clots post-brain tumor surgery is high, so to reduce the risk the stockings are required. Now as a person who doesn’t even like to wear socks to bed, this sounds horrendous! But if it means I don’t get blood clots, well I guess it’s a thing I’m going to need to get used to. I think the next few months are going to be very difficult. A character building experience some might say…
Last day at work - Friday 20th August
Today has been a strange day. It was my final day “in the office”, as I’m stopping work to prepare for my operation next week. I have to admit I’m feeling a little sad about it. Work has been a real safetynet over the past few months. When I needed a distraction from all this, and an “injection” of normality I could always fall back on work. The work isn’t easy. In fact it is incredibly frustrating at times. But that’s part of the distraction. Being able to make plans for the department in the coming years is time consuming and slow, but ultimately very rewarding. I’ve handed over as much as I can and tried to remove myself as “a blocker” from as many areas as I can, but it could be that certain areas stall until I get back to finally drive them forwards. Here’s hoping for a quick recovery and staggered return to “normality”, whatever the hell that is in 2020/2021!
Houston, we have a seizure! - Friday 20th August
Just when Friday wasn’t strange and emotional enough, Gary steps in and makes things worse. 6:30pm rolls around and I’m making a cup of tea in the kitchen. I suddenly feel something “isn’t right”. I’m standing and realise I need to sit down quickly before it happens. I start to walk the few meters across the kitchen to the nearest chair but don’t make it in time. My body goes into a focal (partial) seizure.
As I’m walking I say to my wife: “I need to sit down”, but the words came out slurred (they sounded fine to me). Luckily I manage to lean on the kitchen worktop when it happens, so as not to fall over. I gently start to rock back and forwards, this is out of my control. At that point Claire told me to keep speaking, as it’s good to know what effect the seizure is having on my speech. At that moment I actually struggled to speak. That isn’t through lack of ability, it was through lack of “being bothered”, would be the best way to describe it. There seemed like a real disconnect between myself and reality which I didn’t have the energy or inclination to break down at the time.
The seizure seemed to pass quite quickly. Probably 20-30 seconds in total. I managed to sit down and take in what had just happened. Annoyingly I didn’t feel any ‘release’ of pressure in my head which I’ve had in the past sometimes. I actually didn’t feel any difference at all.
So this was the first clear ‘core function’ seizure I’ve had since the 11th June. There are two intriguing similarities between them: they both happened on a Friday after work, and both happened while coming off steroids. Now this may be a complete coincidence? I have no idea. Maybe I’ll ask the team next week. Next Friday can’t come soon enough!
Time slows down - Sunday 22nd August
I knew this would happen. As soon as I had a date everything would shift. Suddenly time slows down as I’m no longer living each day waiting for a phone call, I’m living each day with a future date on ‘x number of days’ away. It certainly doesn’t help that sleeping is difficult. Only sleeping 3-4 hours a night makes for very long days! I think this may be the longest week of my life. I need to find a distraction (that isn’t work) to keep me occupied. Roll on next weekend and the Belgian Grand Prix. I will never be so happy as to be able to watch a Grand Prix knowing surgery is over!
Cancelled surgery #1 - Tuesday 24th August
So today was a bit of a roller coaster. I woke up very early (I’m still not sleeping too well), as I needed to complete my PCR test at 7am. This works out as 3 days before surgery on Friday. Once completed I went for a little walk to post it in a priority post box. I saw absolutely nobody at that time of the morning, which was handy for COVID. I just so happened to walk past my old secondary school too, which was a trip down memory lane. Not much looked to have changed apart from some of the dilapidated classrooms have been knocked down and replaced with sports courts. I remember them being bad in 1998, I hate to think what they would have looked like 23 years later!
Unfortunately the positive start to the day wasn’t to last. A few hours later I received an email from the hospital stating that my operation on Friday had been cancelled due to a staffing issue with the team. I do wonder if this is all related to COVID, as it seems very strange that an operation planned 1.5 weeks in advance suddenly doesn’t have an important member of the team available. This is disappointing, but in all honesty I’d much prefer they are 100% happy with the team and everyone is available, rather than a ‘settling’ for a team just to get the operation ‘done’. So for the sake of another few weeks (after waiting 4 months), that’s fine by me!
Note that I’ve called this update ‘Cancelled surgery #1’. I’m hoping that there won’t be a #2!
The end of a long week - Friday 27th August
Today was supposed to be the day of my surgery. Unfortunately it was cancelled on Tuesday. In some ways I’m glad it was cancelled so early into the week, as that has given me time to get used to it all. If it had been cancelled the day before, that would have been even worse.
I’ve now been signed off work by my GP until my surgery date. I’ve managed to work for over 3 months, but the combination of the drugs and tumour are starting to take its toll. I can have dizzy spells and get tired very easily. One minute I feel fine, 5 minutes later I’ll feel totally different, almost drugged / drunk (I don’t drink). This all has had an impact on my concentration and work. This is especially true now that I’m off the steroids. They gave a little boost that enabled me to power through, but without them it’s difficult.
So all in all, a very long week. I’ve started making plans for the coming weeks as I’ve been given a very loose date of the 10th September for surgery. It’s not guaranteed, but it’s the only date we have to work towards at the moment, so it will have to do. With the children going back to school on the 2nd September I can see this being an interesting few weeks ahead!
A promising end to the week - Saturday 4th September
It has been a very busy week, lots going on! In preparation for recovery we’ve had a third of the garage converted into an office. This frees up a room that can be used as a spare bedroom. This will be really useful if I need friends and family to stay and help during this period. Because of this, I’ve been gradually cleaning up and making sure we can find things. I can’t explain how frustrating it is not to be able to find tools in the garage. A 5 minute job takes 20-30 minutes just because I can’t find the tools! Saying this, it’s all looking great, not 100% yet, but I’ll be able to potter about during recovery and finish it all off.
My kids are now back at school so I’m self-isolating at my parents. The risk of me getting COVID has jumped since we can no longer control or monitor who the kids are interacting with. Since it takes around 48 hours for COVID to become detectable using a lateral flow test, I could easily catch it and not know about it for a few days. This would be bad in terms of the operation. It puts me at risk, as well as the whole 12-14 people team who will be involved in the operation.
I had some really positive news on Friday when the neurosurgeon who will be forcefully ejecting Gary, phoned me. He phoned for 3 reasons:
To apologise for the cancellation on the 27th. To check on how my seizures are at the moment. To see if I would be interested in taking part in a new feasibility study related to more detailed brain imaging.
In relation to point 1, although this was disappointing, I really appreciate the fact that he made the difficult decision to cancel surgery. It was made because a critical team member wasn’t available. I’d much prefer to go into a long operation with the correct team, than a team pulled together just to ‘get the job done’. This makes me feel more comfortable about the surgery, both from the fact that I know the best team is involved, and also that the neurosurgeon has the team he wants around him. This must be a confidence boost for him too. Not that I expected (or even needed) an apology, it’s nice to be given it. The NHS are doing a fantastic job considering the tidal wave of craziness they have been under for the past 18 months!
Point 2 is an interesting one. It’s been a few weeks since I’ve had a ‘core feature’ seizure, but that doesn’t mean my brain hasn’t tried! There are certain days where I feel quite ‘detached’ from the world. If not ‘detached’, then I can be quite fuzzy headed where concentration is hard. I’m no expert, but this seems to me as though my brain is trying to have a seizure, but the drugs I’m on are stopping it. I keep a detailed seizure log and have been keeping the hospital team constantly updated with how I’m feeling day to day.
There have been discussions this week about upping my drugs, or even putting me on a second drug to try to combat these episodes during the operation. If I were to have one during the operation it could be bad! Although now it sounds like the decision has been made not to change my medication. I’m personally not concerned either way. I’m happy to follow the team’s advice. They are the experts afterall! According to the neurosurgeon it could be that the operation is adjusted to account for these ‘almost’ seizures, this could mean I’ll be awake for less time, which is safer if I do have a seizure. But it also means they won’t be able to take out as much of the tumour because they won’t know if they are inadvertently taking out ‘good’ parts of my brain. Ultimately it’s the neurosurgeon’s decision, and he will be making it on the day. I just need to keep the team informed as to how this week goes. That’s all I can do!
Point 3 is super exciting. I’ve been offered the chance to take part in a new feasibility study related to Fluorodopa PET Imaging in Glioma. I’ll be administered intravenously with a mildly radioactive drug, called fluorodopa. The PET scanner then detects the radiation within the tumour. This imaging should give the team a lot more information about the internals of the tumour that a MRI & CT scan can’t show. So for example, the more aggressive parts of the tumour will show up on the scan, allowing the neurosurgeon to focus on those areas and make sure they are removed as a priority. In this instance the more data the team has the better, so I’ll be consenting to taking part in the study. It’s great to think that these scans could help with diagnosis of tumours in other people in the future. I’m also keeping my fingers crossed that I will also have access to these more detailed scans when I request them all post-surgery.
All in all a very busy week! Next week could be G-day week! We shall see, I expect to hear more on Tuesday, so watch this space. Gary, your days could be well and truly numbered. 6 days and counting (hopefully!).
MRI & PET scan day - Wednesday 8th September
So it’s G-day + 2, and all is still looking good for Friday! I had to sign a lot of forms today related to the feasibility study and the actual operation. It was mainly going over the risks associated with surgery and what to expect. I’ve now been put on a 2nd type of seizure medication to try and head off the last of the seizure symptoms I’m having (pun intended!). My first PCR test came back clear, and I had another PCR test today. I will most likely have another 2 this week. My poor nose!
The MRI scan went well today. It lasted around 40 minutes. Thankfully I didn’t have a reaction when they injected the ‘contrast’ this time which is great. It was loud but tolerable. The doctors and staff at the hospitals (I went to 2 today) were all fantastic. I couldn’t wish for a better team. I feel very fortunate to live in Oxfordshire.
The PET test unfortunately wasn’t as pleasant. It was nothing to do with the fluorodopa, it was the fact that CT scanners really aren’t built for comfort. The scan lasted a whole hour, and honestly it felt like a lot longer as I had no reference point for the time! I was strapped to a machine with my head restricted and my feet were cold. The worst part was that there didn’t feel like there was enough padding behind my head. After 10 minutes the back of my head started to hurt, and once you notice it, it’s hard to stop focusing on it. Especially when there’s nothing else to do! Try it some time, it takes a surprising amount of energy to lie perfectly still for 1 hour while staring at the ceiling. I’m very glad it is now done though. Apparently the scans came out really well and they got all the data they needed for Friday’s operation!
I also found out a little about the surgery itself. I’ll be lying on my left side for the operation with some sharp points tightly pushed against my skin to stop my head moving. I’ll have a cannula in my right arm, as they want me to be able to move my left arm when I’m asked too. Since there’s a risk of partial paralysis on my left side, they will be testing for this throughout the operation. It sounds like this could be quite uncomfortable on my neck which is a worry, but I’m hoping I’m drugged up enough to really know about it!
So anyway, this is likely to be my last update for a little while, as I should be heading into the hospital around midday tomorrow. Fingers crossed Friday all goes well and I’ll be able to post updates soon. This should include the PET scan imaging as well as a before / after image of my brain, minus Gary!
No matter what happens, thanks everyone for all your support, kind messages & visits over the past 4 months. They have been very much appreciated. Here’s hoping the rest of 2021 / 2022 improve!
Thrust into the post-surgery world
So apologies to readers waiting for an update, it’s been quite a few months as I’ve been a little busy in recovery, a lot of things have happened so this is going to be a long update! I’ll pick up from where I left off on what I can only describe as the longest week of my life!
Into hospital maybe? - Thursday 9th September
So Thursday was a very long day. I hadn’t been sleeping well all week, probably due to a combination of drugs and the stress of waiting for the operation. The fact that I was still having seizure-like symptoms didn’t help either. So I found myself awake at 3am thinking what can I do with my time as I didn’t think I’d be able to sleep. So I decided to do something I’d been putting off for months, simply because it isn’t pleasant and not what you expect to be doing at the age of 39 years old. So I planned my own funeral.
My sister is the executor of my will, so I wrote a fairly brief email for her, listing my basic wishes. For example:
- Cremation or burial
- Religious or non-religious
- Music / Dress Code
- Flowers or donations to a (brain cancer) charity
- Budget plans for payment
- Where to spread my ashes
I titled the subject line of the email “Unpleasant email” and used Gmail’s scheduled send functionality to send it at a more sociable time. In hindsight I should have set the subject to ““Unpleasant email [Don’t read in public]”, as I think I caught her a little off guard. It turns out she read it while in the supermarket, which unfortunately made her cry down the bread aisle of her local Sainsbury’s. I found this out in her reply back to me later in the day. The email chain is still difficult and upsetting for me to read even many months later.
So there you have it, learn a lesson from me: When you are sending an email about your funeral to your relatives make sure you consider when and where they might be when they read it! You can use the short checklist above as a starting point for your planning. Depressingly (for a 39 year old) I got much of this information from a checklist on the AgeUK website.
After that I still couldn’t sleep so I wrote a draft “Final” blog post for this very blog, as I’d already arranged for it to be published by a good friend and colleague at work should the worst happen. Thankfully as you can probably tell this preparation hasn’t been needed! On a more positive note I now have an idea of what I want my funeral to be like at the ripe old age of 39!
Let’s move past this deeply depressing section because the Thursday hasn’t even started yet! Due to the COVID risk from my children I’d been staying with my parents for a few weeks. So my parents and I would be making the 1.5 hour journey back to Oxfordshire in preparation for going into hospital later in the day (2pm).
Earlier in the month I’d had multiple phone calls with the team looking after me as to how the days before surgery would go. We had a “Plan A” all the way to a “Plan E”. Plan A was: I’d phone the hospital at 2pm the day before and a bed would be available. Travel to the hospital that day and stay overnight before the operation first thing on Friday morning. Of course nothing ever goes to plan! I phone at 2pm and there’s no bed available and nobody to really speak to about it.
At this point I was in the middle of feeling terrible due to my brain wanting to have a seizure but the drugs stopping it from happening. So I went to bed for a few hours to try and sleep it off. During those hours my wife and eventually my mother tried to get a straight answer from the hospital to see if I would have a bed that night. Around 7pm we got confirmation from the hospital to say that a bed wasn’t available but the operation was still going ahead in the morning. So I’d be sleeping in my own bed the night before the operation and leaving early for the hospital in the morning. In hindsight this was actually a good thing as you will read later in the update.
I’d just like to point out that this isn’t a dig at the excellent work all the NHS admin staff are doing. If there are only a limited number of beds available there’s not much you can do! Especially during Covid, which was on the rise in Oxfordshire at the time.
Day of Days (G-day is finally here) - Friday 10th September (day)
G-day stands for G(ary get the f*ck out of my head)-day. And it’s all a bit of a blur to be honest. I woke up early as again I couldn’t sleep due to nerves. I was hoping to sleep a little in the car but wasn’t feeling well at all. My brain felt ‘fuzzy’, I couldn’t concentrate and had very little energy. I couldn’t have any breakfast due to the operation being in the morning so that didn’t help either. We set off early so as to avoid any traffic. The last thing I needed was to get stressed because we were late!
When we arrived at my home I finally got to see my wife and children for the first time in a few weeks. Covid and cancer really don’t mix well! My wife and I had already decided that she wouldn’t be coming to the hospital with me. She knew she would get upset, which would likely upset me too, which isn’t what you need just before a major operation. So she stayed at home and took the kids to school, to give the impression it was just another uneventful day! They knew that “Daddy was going into hospital to have the lump in his head removed”, but being young didn’t fully realise the seriousness of it all.
I needed to be at the hospital for 9am to be admitted to the ward for the operation prep. Once there nobody was at the reception to admit me so I ended up speaking to another patient waiting there. He was also being operated on today by a different team. He’d already had brain surgery 14 years earlier, the scar was clearly visible on his head where his hair hadn’t grown back. We made small-talk for a while but as we were both nervous it felt quite forced.
The reception staff arrived and admitted me. I had a brief consultation with the consultant anesthetist as he wanted to check I hadn’t eaten anything and wasn’t allergic to any medicines that I knew of. All standard questions for pre-surgery. Interestingly this is the consultant anesthetist who wasn’t available for my previous surgery date due to him being in Covid isolation. I guess the Neurosurgeon has a team that he likes to have around him, especially considering how big my tumour was and how long the operation would be! After the consultation I waited in reception for 5 minutes or so until one of the team led my mom and I to the bed I’d eventually be in after surgery.
The other patient who I’d been speaking to was in the bed opposite. Knowing that I wasn’t on my own my mom left and went back to the car where my dad was waiting to take them home. It all happened so quickly we both said our ‘final’ goodbyes and that was that. I was more worried about her getting lost in the hospital than the actual operation at that point.
Now I’d only been on my own for 1 or 2 minutes and the nurse came in to start pre-surgery prep. She took my blood pressure and oxygen levels etc. Then I had to put on what would quickly become the bane of my life for a month: Deep Vein Thrombosis (DVT) leggings. The reason for wearing these is that stats show that after brain surgery you are 30% more likely to develop blood clots which can be fatal if they travel to the heart or brain.
Once prepped I got to meet my Neurosurgeon for the first time in person, he introduced himself and checked I was doing okay. Usually I would have shook his hand but due to Covid I didn’t think it was appropriate. You’d be surprised how much a little thing like that annoyed me. You’re about to put your whole life and future into this person’s hands and you can’t even thank them with a handshake.
The Neurosurgeon left, and before I knew it I had a group of people around me leading me down to the operating theatre. I said goodbye and ‘good luck’ to the other patient in the room and out of the ward we went. I have to be honest I don’t remember the walk to the operating theatre at all, or what we discussed on the way there. My brain was just trying to take in the enormity of the situation ahead of me. After 6 months of mentally preparing for this moment it is finally here!
We entered the side room to the operating theatre and the team started to work on me. They told me to get up and sit on the trolly in the centre of the room. I distinctly remember thinking “This could be the last thing I ever do as a person”, It took all my courage to get onto the trolley and I have to say it’s the scariest thing I’ve ever had to do in my whole life. There were 3-4 people in the room prepping me, for the most part I had no idea what they were all doing or saying to me. But I do remember them marking the right side of my neck with an arrow pointing up to my head in black permanent marker and then them telling me they would be putting a cannula into my right hand, then once done they would put me to sleep and put something called and Arterial cannula directly into my artery in my right arm. They also put 2 other cannulas into the top of each of my feet. I’m very glad they did all this while I was asleep as I hate cannulas at the best of times! The last three sounded deeply unpleasant.
So that was that, cannula in the right hand, they said they were injecting me with anaesthetic and it would feel cold running up my arm and that I may have a strange taste in my mouth. I felt the anaesthetic reach the right side of my neck and I passed out.
During the time I was passed out the team prepared me for surgery. I was moved onto my left hand side and my head was placed in a metal contraption with 4 very sharp points sticking into my skin; these were to hold my head in place for the operation. The team cut the skin on the top of my head and peeled and folded it forward to expose my skull. At this point they then used some sort of medical saw to cut through my skull and expose my brain (and Gary) The incision started at the front of my skull just after my hairline and travelled backwards right down the centre before turning to the right and coming back to just before my right temple in a large horseshoe shape. They’d basically had to remove the right hand side of my skull due to the sheer size of Gary (the prick). Thank goodness for anaesthetic and anesthetists is what I say!
Once all this was done they reduced the anaesthetic and used other drugs to bring me round. I remember waking up lying on my left hand side, my head was already open and I couldn’t move, there was a large transparent plastic cover in my peripheral vision to the right just above me (like the plastic covers you see on children’s buggies to protect them from the wind and rain). There were 2 people in front of me and a television screen just behind them. One person was the consultant anesthetist just watching proceedings, as I guess he’d done most of his job and was just monitoring the situation. The other person was a lady. She was the Neurophysiologist looking after me, her job was to be the go-between between me as a patient and the Neurosurgeon. She’d ask me questions and update him on how I was reacting to those questions.
Then the last thing in front of me was the TV. It had live pictures of the inside of my head, now they weren’t gory pictures with lots of blood and bone etc. They were the 3D scans of my head taken from my last MRI scan. The crazy thing I remember is they updated in real-time, I could see exactly where the Neurosurgeon was putting his tools. There was no pain while he was doing this but I could feel a distinct “pressure” inside my head that I’d never felt before, so I knew he was there.
I remember finding the real time 3D imaging fascinating. When they gave me the chance to ask them questions I remember asking them how it all worked. I was thinking it was some sort of haptic technology driven tool but it turns out it was a lot more clever than that. The team had placed 3-4 sensors on the outside of my skull which could detect the “marking tool” the surgeon was using inside my skull. By monitoring the input from these sensors they could get a computer to update the screen in real-time, even for a person who works in technology on a day-to-day basis this blows my mind!
So what exactly were they marking in my head? Well it turns out this is where the PET scan that I’d had on Wednesday comes in. The feasibility study in theory should be able to be used to identify the different cancer grades within the tumour, something that an MRI / CT scan on it’s own can’t show. You can see the results of my PET scan below:
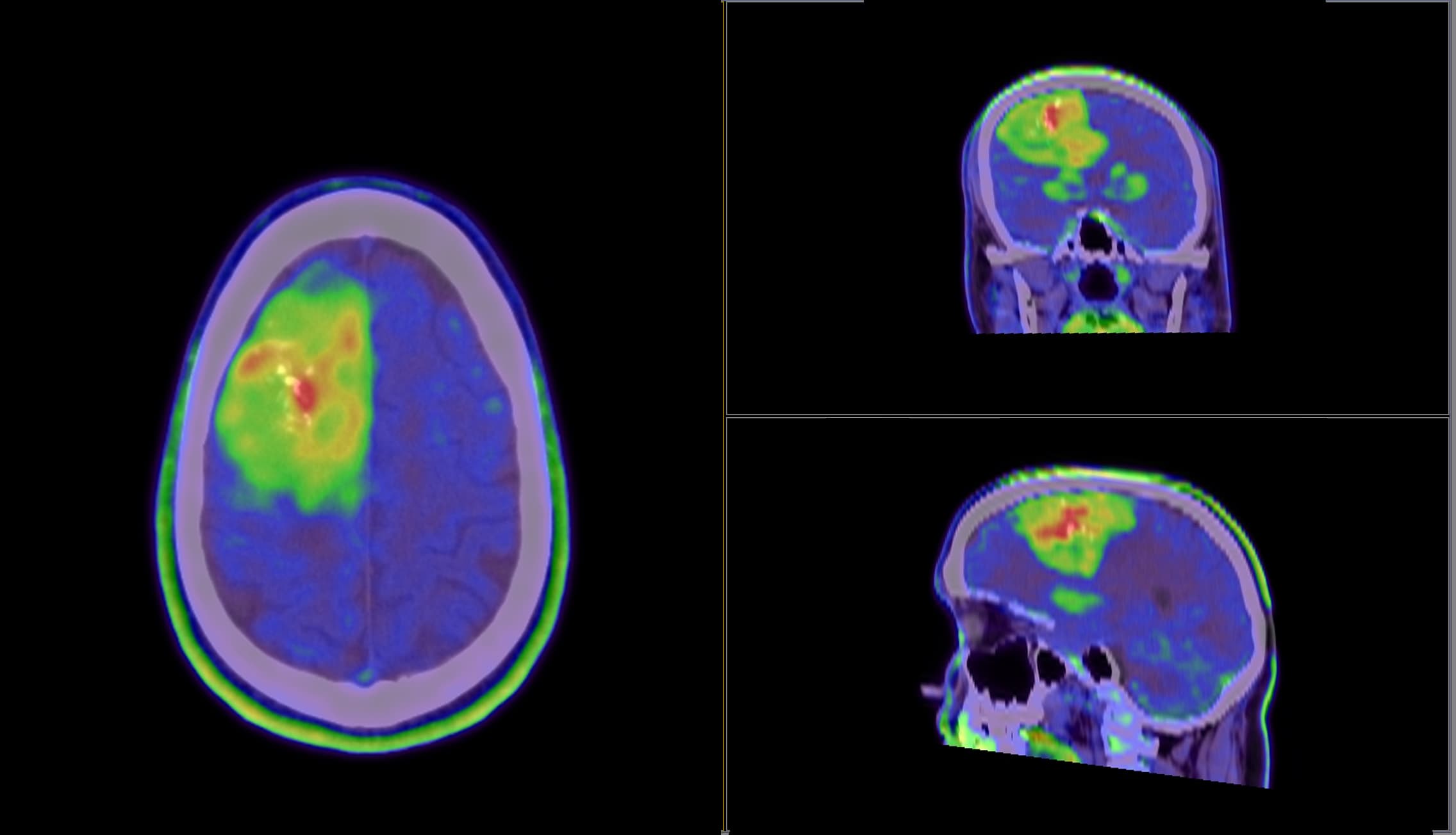
Now this is an ongoing study and I’m one of around 30 patients in the trial. The final results of the study won’t be known for many years. The above image is the result of the hour-long scan I had to endure. The radioactive isotope was absorbed by Gary, then depending on the grade, different parts emit radiation at different rates. This Is then picked up by the CT scanner resulting in the image above, hence showing Gary’s internal structure. My assumption is that the red areas are the higher grade (e.g. grade 3), through to green / yellow being lower (e.g. grade 2). But this won’t be known and confirmed until the study concludes in a few years.
The reason I’m telling you this is because when I woke up I heard the team were having a conversation where they were talking about colours and numbers. As it turns out the team were talking about these scans. They’d identified certain areas of Gary that they would like to biopsy for further analysis, before moving onto removing Gary completely. I think because Gary was so big there was a treasure trove of data for the study! I heard from the team post-surgery that they removed 8 areas of Gary for further analysis. They would have liked to have taken more but the Neurosurgeon put his foot down to say no more, as the procedure with only 8 added 1-1.5 hours more to the surgery time. One thing I remember finding amazing was how the whole team was working together. The Neurosurgeon was working inside my head but he obviously couldn’t see the real-time scans with the areas he was supposed to be removing, so the team were speaking to him telling him to move left / right / up down etc. Only the language they used was more medical than that, so using more medical references from the brain. It was incredible to see and hear.
I remember asking a few more questions about what was going on that the Neurophysiologist couldn’t answer and getting the response “that would be a question for the Neurosurgeon, but he’s a little busy at the moment!”. Then I think they put me to sleep again (probably to shut me up to be honest!). I’ve been told there were between 12 - 14 people in the operating theatre at the time but I only remember seeing 2 people and hearing the Neurosurgeon. The other folks must have been supporting the Neurosurgeon “above me”.
The next thing I remember is coming to, my eyes were closed so I couldn’t see anything but I could feel they were stapling my head back together. I felt no pain but I just remember the pressure of the staple gun reverberating through my body. I also remember thinking “that’s a lot of staples!”. If you’ve ever used a staple gun you will know that you have to put quite a lot of pressure on the handle before the staple is released. Well it sounded exactly like that, only into the top and side of my head around 95 times!
Annoyingly that’s all I really remember from the surgery. I estimate maybe 45 mins to an hour of the 7 hour operation. I’ve actually been quite disappointed that I don’t remember more of it and nothing more has come back to me over time. A couple of weeks after surgery I spoke to one of the Neurosurgeons who was also in the operation helping, about this. And she said that this was intentional. They constantly increase and decrease the drugs throughout the surgery as there are certain unpleasant things they don’t want you to remember. So I’m thankful for that, but in another way I will always wonder what happened in those 6+ hours of my life I can’t remember!
Recovery starts - Friday 10th September (evening & night)
The next thing I remember is waking up on the hospital ward with the absolute worst headache I’ve ever had, not really surprising when they’ve just removed approximately 15% of my brain matter! I could barely move and had to sleep upright due to the pressure lying flat would cause.
I’m so glad they put me to sleep before inserting the Arterial Cannula, as the bruise I had on my right arm was huge! It must have been quite a struggle to get it in there!
Now I have to be open and honest. This was the worst night’s sleep I think I’ve ever had, hence why I was grateful I slept at home the night before. I’m not a fan of hospitals anyway, but this night will stay with me forever.
Due to the risk of blood clots I had my DVT leggings on, but as an extra “brucie bonus”, I also had a pair of leggings that inflated & deflated every 10-30 seconds. The only way I can describe it is when you go to have your blood pressure checked and the strap on your arm inflates then deflates. Well imagine that on the total length of both calves. Inflate / deflate all night long every 10-30 seconds!
I also found I couldn’t really move both because of the leggings and the pain it caused in my head. I found my legs were roasting hot but my top half was cold because I couldn’t pull the blanket up over myself. What made things worse was I couldn’t find the call button to ask for help. I must have spent 20-30 mins looking for it before I eventually found it (it may not have been that long but it felt like it!).
Just to make things worse the patient opposite me who I’d spoken to before surgery was being violently sick all night. I think he must have had a bad reaction to the anaesthetic. So yes, all in all a terrible night’s sleep 0/10 would not recommend!
Let’s get the hell out of here - Saturday 11th September
After that one night in hospital I was absolutely determined to not have to stay another. So once it was light the nurses brought around food that I couldn’t eat. Everything tasted strange from the anaesthetic. I eventually managed to eat dessert, which was a rhubarb crumble with custard. The inflating leggings were taken off so I could finally move my legs. At that point I realised I had a much bigger scar than I expected so I wanted to go into the toilet to take a look. The toilet was only a few meters away but it felt like miles. I asked for a walking frame so I could get there myself but I had to be escorted for the first few times. Looking in the mirror was a weird experience. I couldn’t see the scar at the moment as it was covered in a blue gause, but it was a hell of a lot bigger than I expected. I’m not sure why I thought it would be smaller looking at the size of Gary. How else were they going to extract the prick?!
At the same time as looking at my head for the first time, I managed to brush my teeth! But no matter how much I tried I couldn’t get the weird taste of anaesthetic out of my mouth. Eventually after what seemed to take an age to do these small things I was escorted back to my bed, mostly under my own steam (with a walker).
Next came something that would be a thorn in my side for the next 3-4 weeks. Lying down or sitting up caused terrible pain in my head. This is because, unlike pretty much everyone but medical folks would know, when you get up / sit up / lie down, the intracranial pressure inside your skull changes. Usually you’d never notice this, but when someone has just removed a huge chunk of skull and stapled it back on, you suddenly feel it!
It seemed to take me ages to lie down on the bed but I eventually managed it and got comfortable. But I was determined not to have to stay another night in the hospital so I decided I needed to get moving. Over the next few hours I kept getting up and down again and used the walker to move around the ward. Once I was steady on my feet the nursing staff were happy to let me walk on my own (it was more of a shuffle really!).
At 12pm the nurse came over and said my wife (Claire) would be visiting in the next couple of hours, this perked me up a bit. It would be good to see a familiar face after what had felt like weeks since the previous morning! Claire was very surprised when the nurse mentioned that I was already up and walking about the ward.
2pm came and my wife brought in some M&S chocolates and she got to see my humongous scar. Thankfully I’d had no memory loss, but I was finding speech and concentration very difficult. I don’t think we said much. I think I was mainly staring off into space or at the ceiling wishing the pain in my head would go away. The only painkillers I could have were paracetamol, none of the good stuff I’m afraid! Thankfully they took the edge off the pain. After an hour it was time for my wife to leave. She said she would be back to see me again tomorrow. But I had other plans.
Claire phoned my parents after leaving the hospital and pretty much said there is no way I’m going to be released from hospital tonight and it will most likely be Monday. So my parents stood down from coming to pick me up since they were a 1.5 hour car journey away. But during this time one of the senior doctors came to see me. He said that as long as I’m up and about moving we could try and get a CT scan sorted to check everything in my head was okay and try to get me discharged. I jumped on that in a flash!
I had to wait an hour or so for the CT scan then the porter came to wheel me across to the other side of the hospital. The CT scan took 10-15 mins or so then they took me back up to the ward. It was around 30-40 mins later that the same doctor came to see me and said everything looked great, so if I wanted to he’d be happy to discharge me. I obviously said yes, and he went off to pull together my discharge paperwork (which would take a couple of hours). I immediately tried to phone Claire but I had a slight weakness in my left hand, and I also found that the phone didn’t make as much sense as it had done the day before. Things hidden behind icons were difficult to find. I found this very worrying considering how easy it was just a single day before. But I eventually managed to work out how to use the phone and rang her. At first she couldn’t believe they were discharging me as I was still slurring my speech down the phone. Somehow I managed to get her to believe me with the help of one of the nurses who overheard via speakerphone. So it was then arranged that my parents would travel down to pick me up from the hospital and take me home. This eventually happened around 10pm. So from admission through surgery to discharge I’d been in hospital for 36 hours! That’s pretty crazy when you think about it. 15% less brain and out in a day and a half! To give you an idea of how busy the hospital was at the time, I heard the nurses discussing the next patient who was going to take up my bed once I’d been discharged! The nurses really are unsung heroes, day in, day out working with sick patients, and it isn’t easy work at all!
I don’t remember any of the journey home, but I do remember that the car was really low and difficult to get into especially given all the staples in my head! I don’t think my parents had a very good night’s sleep that night. Mine wasn’t perfect but it was 1000% better than the night before. I still had to sleep at an angle for another few days which was uncomfortable but atleast I wasn’t in hospital!
How does the TV work? - Sunday 12th September
I woke up early as I was in pain and uncomfortable. The F1 Italian Sprint race had happened on Friday during my operation so I wanted to catch-up on what had happened. My Dad had recorded it on Sky+ so before they woke up I decided to go downstairs and try to watch it. Unfortunately, I couldn’t work out how to use the Sky box. I was able to turn it on and find the recordings but when I played them it wasn’t the Formula 1, it was the Formula 2. This totally confused me because the thumbnail preview was showing a Formula 1 car. I tried multiple times to get to the F1, but had no luck. Eventually I gave up and used my phone to watch the highlights on YouTube. This was the start of an ongoing theme over the next few days. Things that had seemed so simple and obvious only 2 days before I was suddenly struggling with. I had the same issue with the Netflix User Interface. I found it too busy and confusing to use. For a once technically proficient person I found this genuinely scary. Thoughts of “how exactly am I going to do my job” if I’m struggling with these simple things! Not fun, and quite a contrast to me only 2 days before. It really did give me some insight into the importance of making things simple and understandable for users that are less technically proficient. If only every web development team could have similar brain surgery. I think we’d have a much more user-friendly internet if so.
Is my head leaking? - Monday 13th September
Odd title I know, but I woke up on Monday and found spots of red transparent liquid on the white pillowcase I’d been sleeping on. Further to that I was certain I could feel “movement” underneath the blue gauze which covered the staples in my head. When I felt something drip onto the bridge of my nose, I immediately got in contact with the Neuro-Oncology team via email to let them know. Within 5 mins they’d got back to me via email and a phone call. They asked me to come back to the hospital as quickly as possible. Of course I was 1.5 hours away at my parents so it wasn’t as simple as that. So I quickly packed a bag of clothes just in case I needed to stop overnight and we headed back along the motorway to the hospital.
Once we got there I waited with Claire who’d met us there for 5-10 mins and one of the Junior doctors took us into a side room and started to remove the staples from my gauze so they could get a better look at my head. She explained that if it was that Cerebrospinal Fluid (CSF) or “brain juice” (as I liked to call it) was leaking from the wound it also means that things can get into the wound / my skull. If this happens it can cause an infection, leading to a whole host of other issues that may even require more surgery. So it’s best to get it checked out. The Junior doctor couldn’t find any obvious leaks so she consulted one of her more senior colleagues. He came to see me and also couldn’t find any obvious leaks. So he decided to do a very scientific test to make sure. He placed a white absorbent pad on my head (like a kitchen towel) and then had me cough and lie down on the bed. This increases the intracranial pressure inside the skull (I know because I could feel it!) and if there’s a leak CSF would come out of the wound and be seen on the absorbent pad. Thankfully nothing was seen on the pad!
The senior doctor was certain the movement and liquid I’d felt / seen was the petroleum jelly (think Vaseline) used to keep the wound moist and clean. My warm head was heating the jelly, turning it to liquid and it felt like water (because I couldn’t see it to verify it wasn’t). He did leave me with a nice vision: Saying that if I do have a CSF leak it would literally be pouring down my face, and if this were to happen phone the emergency services immediately. I’m pretty sure I’d have done that anyway, but it’s always good to know I guess!
With the panic over I headed back to my parents to continue my recovery, with hopefully less drama moving forwards!
General struggles - Tuesday 14th September
So I’m not going to give a day by day update on what happened as it’s very boring and tedious. It felt like a long time for me because I was obviously living it, so to write about it would be even worse! But here’s a summary of some of my general post-surgery struggles I had.
The DVT leggings were terrible to wear. I hate wearing socks to bed and now I had to wear these really tight leggings over my lower legs for a month! They were a pain to get off and it took help from both of my parents to get them back on. I guess it’s a small price to pay compared to fatal blood clots!
As mentioned before, sitting up and lying down was painful. Basically going from 0 to 90 degrees and vice-versa caused a terrible pain in my head, so I tried to avoid moving, but you’d be surprised how often you make these movements going about your general day-to-day life! This was the same for coughing, laughing and sneezing, all these increase the intracranial pressure in the skull. Everytime i sneezed it felt like the top of my head was about to split open!
Related to the above issue, lying down and getting into bed was a chore! I remember having to get up in the night to go to the toilet, then getting back into the bedroom, and it literally took me 15-20 minutes to pluck up the courage to lie-down on my pillow to go back to sleep! I knew that it would only take 2 seconds to do it, but when I also knew it was going to hurt, my brain and body refused to move. I just ended up rocking backwards and forwards on the bed for minutes at a time, hoping the momentum would carry me forwards and I could then go back to sleep.
A strange one but due to the fact that I’d had open-head awake surgery, when they close your head it’s impossible to remove the air pocket that is leftover. So for 6-8 weeks I had a huge air pocket at the top of my skull. And everytime I moved my head I could feel this air pocket move around my head. It wasn’t uncomfortable, it was just weird. It was a similar sensation to someone lightly brushing the top of your head. There’s nothing that the doctors can do about this, it just takes time for your body to naturally replace and recycle the CSF around the brain every 6 weeks or so. So the air was gradually reabsorbed back into my bloodstream. But this sensation lasted 6-8 weeks after surgery, maybe even more.
Related to the air in my head, I could feel my nose randomly “creaking”. It’s hard to describe but it felt like small air bubbles at the top of my nose releasing. I think it may have been related to the CSF fluid redistributing itself and the pressure inside my head stabilising itself over time. This lasted 2-3 months after surgery.
I had to keep the 95 metal staples in my head for 2 weeks and in this time I kept having phantom movements on the outside of my head. Almost like my body was realising that there was a foreign body (or 95 of them) attached to the outside of my skull. This stopped as soon as the staples were removed and the wound started healing.
And finally I think I may have been suffering from something called Abulia. This is described as “a state of diminished motivation”. Now this is a self-diagnosis not from the doctors, but from reading up on the symptoms it certainly seems like what I was suffering with, at least in the first 3-4 weeks anyway.
All in all I think I’ve got off quite lightly considering the size of the scar and the size of Gary. The struggles above weren’t pleasant but they were manageable. I’m very surprised how few headaches I’ve had. If I were to have guessed what the most likely result of major brain surgery would be it’d be headaches. But apparently not. At Least in my case anyway!
It’s also worth noting that the only painkiller advice I was given post-surgery was to take 2 paracetamol! So remember that the next time you have a headache. Paracetamol are so good they even work for folks who’ve had 15% of their brain matter removed!
Biopsy results - Tuesday 21st September
As with most things happening in the NHS at the moment teams are extremely busy. So I wasn’t expecting anything from the hospital on this day until I received an email at 9am asking if I was free for a call with my Neurosurgeon + team at 12:30pm. I replied back and accepted, I mean It’s not like I had much else on! I wasn’t quite sure what the call was about so really wasn’t mentally prepared for it at all.
I jumped on the call with the team, my wife and parents were listening in too. My Neurosurgeon, never one to mince his words, immediately spoke and came out with the biopsy results of Gary, the now (mostly) evicted prick! He told me the team had managed to remove a whopping 95% of Gary, but the biopsy results had come back to say that some parts of him were Grade 3, rather than Grade 2. Grade 3 are called anaplastic oligodendrioglioma, these are malignant (cancerous) and can be fast growing. And because of this I’d need to start a 6.5 week course of radiotherapy within the next month, followed almost immediately by a 6 cycle course of PCV chemotherapy which will last approximately 7 months. As I’d experienced previously with my Neurosurgeon there was no warning about this news, no “are you sitting down, brace yourself”. Just boom, you’ve got Grade 3 brain cancer! Well you may as well pull off the plaster quickly and get it over with I guess! In hindsight I was expecting it to be a multi-grade tumour even before they told me, I mean why would they have been wanting to biopsy multiple areas in the surgery if it had all been a single grade tumour?
After the initial shock, I managed to compose my thoughts and asked a few questions about the surgery itself. I asked if there’d been any nerve damage at all, as I had a slight weakness in my left hand. He looked slightly bemused by this and said no there’d been no nerve damage and the operation had gone very well. It turns out there’d been a slight miscommunication from what was said to Claire immediately after she got the phone call from the Neurosurgeon to say surgery had gone well and that I was in recovery.
I was led to believe that they stopped surgery because they had caused slight nerve damage. But this wasn’t the case. It was actually that if they went any deeper it could have caused nerve damage, so they stopped. I later found out that the team were using a technology during the operation called Neurophysiology. This involved strategically inserting 5-8 metal pins into the left hand side of my body and monitoring the signals from these pins as they fired electrical impulses into my brain. It was basically a type of automated testing to see when they were getting close to nerves that actually did something, rather than just prodding Gary the useless prick. So once the safest amount of Gary had been removed, the team decided I was getting very tired and I needed to save my strength for recovery. So that’s why the operation only lasted 7 hours!
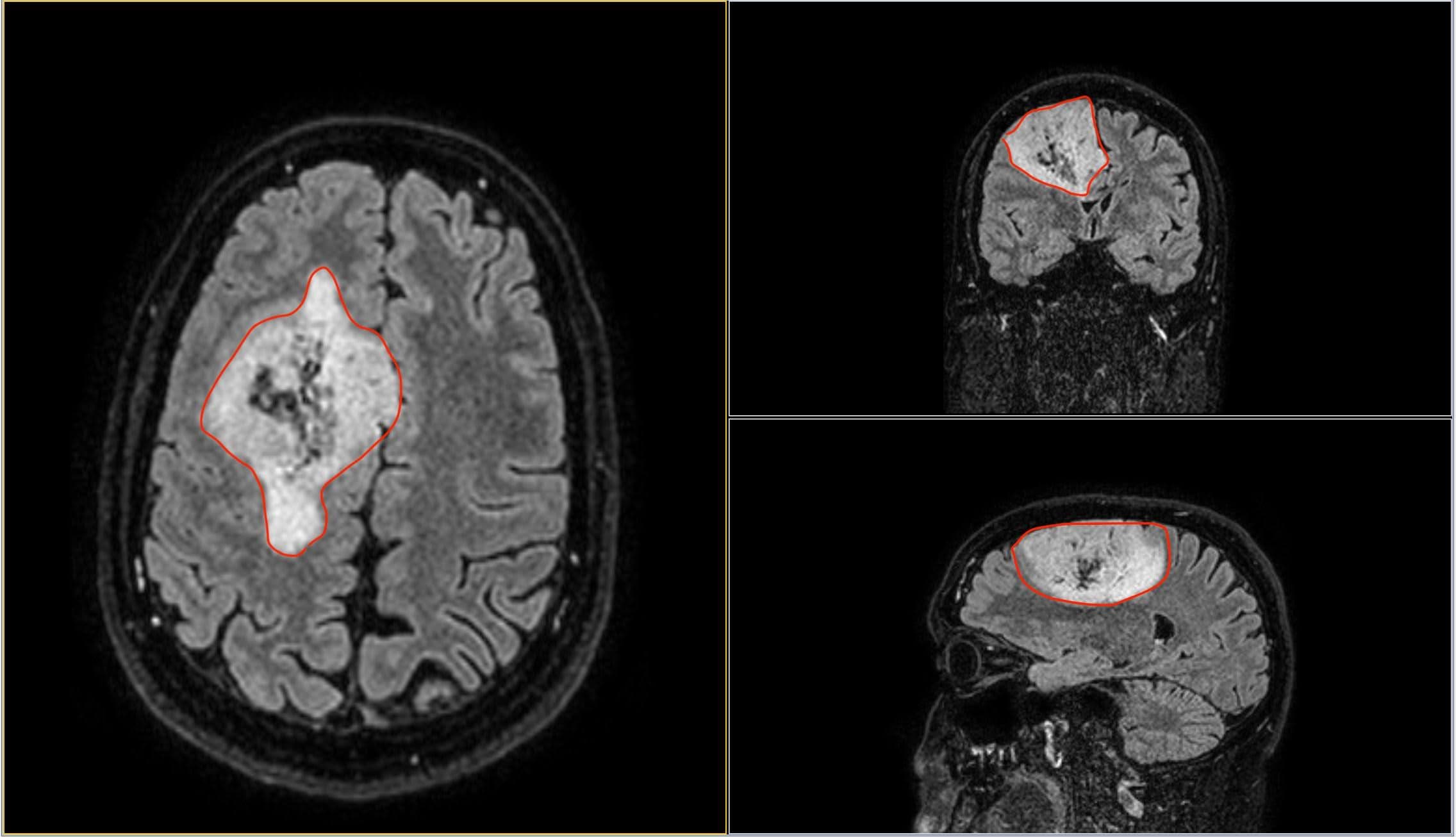
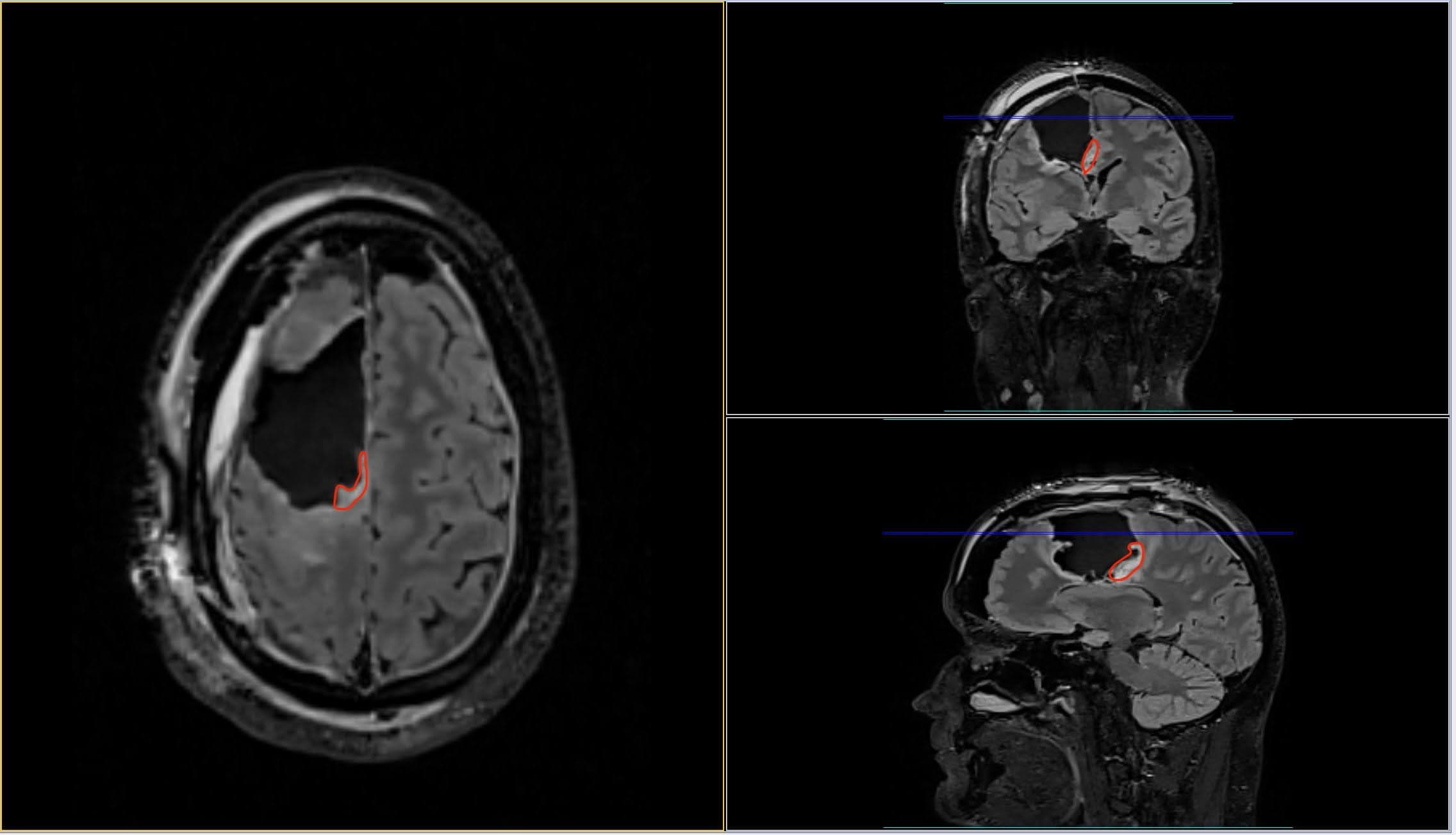
In the above images you can see the before at the top then the after scan of my brain with Gary highlighted in red. As you can see he’s mostly gone apart from some left over in the deepest part of my brain. This leftover is what the Radiotherapy and Chemotherapy are going to be targeting as well as any residual cancer cells around the edges of the surgery.
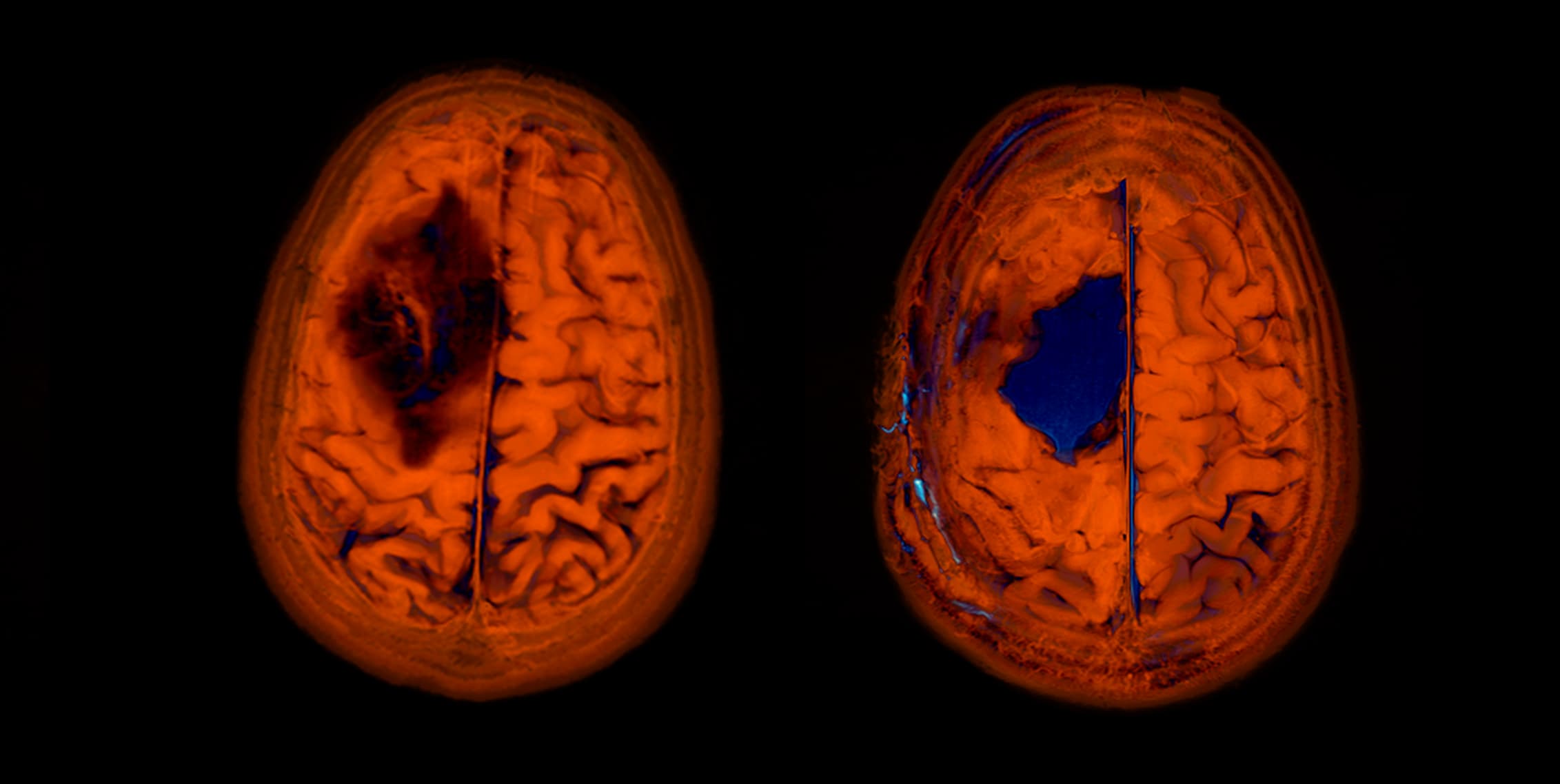
Now a question I’ve been asked many times off the back of the quite frankly incredible image above is “what happens with the hole moving forwards?”. Well this is a question I asked back when I was first diagnosed and they described the operation to me. The hole will now alway be there. Brain cells don’t grow back. Over time it fills with CSF, but it will always be there. And a fascinating observation I’ve noticed since the operation is I can hear the cavity where Gary used to reside in my head. This is especially true when I’m in the shower and I run the water over my head. The right hand side of my head sounds hollow compared to the left! I like to compare it to looking for a stud wall behind some plasterboard. As you tap on the plaster the sound changes from hollow to dense. It actually took me a while to work this out and what was different when I was having a shower in the mornings. It’s a strange feeling to know there’s now just a big hole in my head!
After the appointment I didn’t have long to wait as my initial appointment with the Oncology team to discuss the radiotherapy as it was set for the following day. No time to waste with Grade 3 brain cancer I guess!
Further treatment appointment - Wednesday 22st September
The whirlwind that my life had become continued with a meeting at a new hospital and a whole new team of experts. The meeting was to discuss the post-surgery treatment I was signing up for. This meeting was mainly about radiotherapy, with the chemotherapy discussion coming at a later date.
There were 2 oncologists and a number of nurses in the meeting as well as my wife. I’d made the decision that whenever something important was being discussed I should always have company as I knew for a fact I wouldn’t remember it all, since it had only been 12 days since my surgery! There was no chance of me remembering much!
The meeting seemed to last ages and there was so much information being discussed I found it hard to concentrate on what was being said, so I’m very glad Claire was there with me to take notes and remember everything.
As well as introducing the timeline for the radiotherapy all the wonderful side-effects were discussed too. And they always seem to save the best (and rarest) to last, which includes the fact that radiotherapy in some cases can lead to other forms of cancer. What’s better than having 1 type of brain cancer? Well 2 forms of brain cancer I guess!
Once all the difficult conversations were discussed, I signed on the dotted line to say I agreed with the treatment. I’d already decided this was the direction I wanted my treatment to go even before hearing all the side-effects so it wasn’t a hard decision to make.
With a room full of doctors and nurses I decided to ask the question if it would be possible to take the staples out of my head. It was coming up to 2 weeks since surgery and this was close to the date they had said, so I may as well have it done while I was there anyway.
I felt quite sorry for the nurse when she saw the sheer number of staples in my head. I wouldn’t even know where to start. The technique involves taking every other staple out first, just in case the wound hadn’t healed. I guess they don’t want your head to suddenly open up again, and every other staple allows for some support while assessing the wound. Removing the staples wasn’t as uncomfortable as you’d expect. There were a few minor sharp pains with a few of the staples, but most of them were pain free. Because there were 95 of them it seemed to take ages!
Once the staples were out I was done for the day and I was travelling back home to be with my wife and children. I also managed to wash my hair / head for the first time in just under 2 weeks. It was the most amazing shower and I actually felt a little more human after it!
My kids were at school when I got back, and I needed to sleep for a few hours. This was the first time they’d seen me since before the surgery so it was going to be interesting to see how they would react to the huge scar on my head. My youngest son wasn’t phased at all but as soon as my eldest saw me I could tell he wasn’t comfortable with my new Frankenstein’s monster look. We tried not to make a big deal of it but I ended up having to wear a hat around the house for a few weeks while my head healed to stop him freaking out.
Prognosis
So jumping back to the meeting with the team they went over the scans and some of how well the surgery had gone and then got down to the nerve-racking part, which is the future prognosis. They could only give me timescales for the “average” patient in my position. It was mentioned that this isn’t a cure and it’s likely to always be there.
The timescales they gave me are below:
- Do nothing - the average patient can expect to live 7 years
- Radiotherapy followed closely by chemotherapy - the average patient can expect to live 14 years
So here’s hoping I’m the exception to the rule or not the “average” patient. Else I certainly won’t need to worry about retirement plans (that’s probably a blessing actually)! Given the retirement age for men is 68 in the UK, I’ll fall some 15 years short. But a lot can happen in 14 years, you never know with further funding and research more options could be available by then!
Making my mask - Friday 1st October
Because Radiotherapy is a very targeted treatment, they need to make sure the treatment area is accurate for every session, and this involves me not moving my head at all for around 6-8 minutes while the treatment happens. This of course is impossible without aid, so they make a fitted mask that you wear throughout the treatment, that you can then take home should you wish to at the end!
The mask is made by heating up a rubber mesh to around 70 degrees centigrade in what looks like a pizza oven. While you are lying on the “couch” they quickly pull the heated mesh over your face / head and manipulate it a little to make sure it fits snugly. Then you have to wait 20 minutes underneath it while it cools, before it can then be taken off.
It’s a very strange sensation when they first pull it over your face. It’s like someone is pulling a plastic bag over your head and for the first second or so there’s initial panic in that you think you can’t breathe. But once you breathe through your nose it’s actually quite pleasant and warm. You also need to close your eyes so as to not pull out your eyelashes when they remove it. A side effect of this means that during the treatment itself you have no idea what is happening around you.

It’s also worth noting that when I say you lie on a “couch’’ it’s not like something you sit on to watch TV. It’s actually a flat carbon fiber board that isn’t built for comfort. It’s built for accuracy.
Radiotherapy Starts - Tuesday 19th October
The radiotherapy happened over 6.5 weeks, with 33 sessions in total. I needed to go into the hospital everyday apart from weekends. The actual treatment only took 8-9 minutes once I was in the room. It was the travelling there and back (~45 mins each way), plus there was sometimes a wait for the machine to be ready, as there were sometimes delays with other patients. The worst day I had was one particular Friday where I left the house at 8am and used the NHS hospital transport. My treatment was delayed by 1.5 hours, so I missed my transport slot to go home. I eventually got back at 14:30 and was absolutely shattered.
I’d got into the routine of having the treatment, coming home, eating, then going to bed for 2-3 hours. Because of this I was so tired, there was no way I could do anything really for 6.5 weeks. The effect of the treatment was cumulative, so as the weeks went on I got more and more tired.
I’m not going to cover each day, but will give a week by week blow of the whole experience.
Week 1: 19th - 22nd October
This week was mainly getting used to the schedule of how it all worked, signing in everyday, waiting in a particular area, hoping that there wasn’t a delay on my particular machine etc. It’s incredible the cognitive load that the “unknown” puts on you. But once into the routine it was fine. The only real side effects I had in the first week was tiredness, and getting used to staying perfectly still when I had the mask on. It was also trying to get used to the machines and what exactly they were doing. As mentioned earlier, My eyes were shut for the whole process so I had no idea what exactly was happening around me for 8-9 minutes, I only had the sound of the machine to rely on. For my first couple of sessions it felt like the whole machine was rocking backwards and forwards because I had no point of reference. With my eyes shut and touching nothing but the “couch”, as soon as your brain thinks you are moving it is very hard to stop it from thinking it! Trust me I tried multiple times! I’m just very glad I don’t suffer from claustrophobia because if I did the whole 6.5 weeks would be a nightmare as that mask was very tight! Sometimes so tight it left an mesh imprint on my nose and forehead.
Week 2: 25th - 29th October
Week 2 was mainly travelling in and out via hospital transport so the days were long and it very much started to feel like “groundhog day”. The funny thing about Hospital transport is the drivers are all volunteers, some were very chatty, others wouldn’t say a word for the whole journey. I often found the drivers were chatty on the journey back, when I was tired after hours of being at the hospital. Small talk is difficult at the best of times, but 6 weeks after major surgery and radiotherapy it is a struggle! The main side effect from this week was I noticed I’d started to get a distinctive tan on my forehead from the radiation. It was like going on holiday without all the fun.
Week 3: 1st - 5th November
Week 3 was a tough week. The whole process was getting very repetitive and I was only just getting to the half-way point! This is also the point at which I noticed my hair was starting to fall out.
I was having a shower one morning and realised there was hair in my mouth. I quickly spat it out then a few seconds later realised there was hair in my mouth again. It was only when I washed my hair I noticed whole clumps of hair were coming out from the inside of my scar. I’d been expecting this as they’d warned me about it, but in the back of my mind I thought it may not happen to me. So it’s still quite a shock when it does happen!
Week 4: 8th - 12th November
Groundhog day continues and I notice more of my hair is falling out, this time from the other side of my head. I guess because of the geometry of how they are targeting Gary, they are hitting it from multiple angles. So I ended up having hair at the back and sides of my head and very little in the middle, with a small patch of hair right at the front of my head. It looked ridiculous so I decided to shave my head completely. This completed my full on “cancer look”, and it certainly shows off my scar a lot more!
The one thing I notice is how much colder my head actually is! You wouldn’t have thought such little hair would make a difference, but it really does! Thankfully I have a few hats that I wore both inside and outside the house.
Week 5: 15th - 19th November
At this point I’m well and truly over the whole process. The journey in and the appointment takes up the whole morning, then I’m sleeping in the afternoon. So by the time I wake up it is already getting dark. So the day is gone and I’ve got nothing to show for it. So incredibly frustrating!
Week 6: 22nd - 26th November
Thankfully getting closer to the end of the whole process now, but I’m starting to feel incredibly drained. It got so bad at the end of the week that on Friday Claire had to phone the emergency number as I felt like I was about to have a seizure. This is something they had warned us about but I hadn’t had any seizure-like symptoms since before surgery. After lying down in a dark room for an hour or so and taking some extra medication that the oncall oncologist had recommended I felt a little better. But it felt depressing, as it was almost like I’d regressed weeks rather than moved forwards.
Week 7: 29th November - 2nd December
The final week! In the weekly Tuesday consultation with the consultant / senior nurse, it was decided that I was going to be kept on stronger seizure medication in the evenings for the foreseeable future. Thankfully I haven’t had any huge side effects on this drug so I didn’t mind. As long as it keeps the seizures away!
Radiotherapy Ends - Thursday 2nd December
In my final session on the Thursday I took a whole bag full of chocolates in for the nurses and reception staff as they’d all been so helpful and friendly for the past 6 weeks. They seemed very happy with them. I guess they must get it quite a lot. Since it was my final session I asked if I could film my radiotherapy session as I was curious as to what exactly the machine was doing, having had no idea for the past 32 sessions. Thankfully they allowed it.
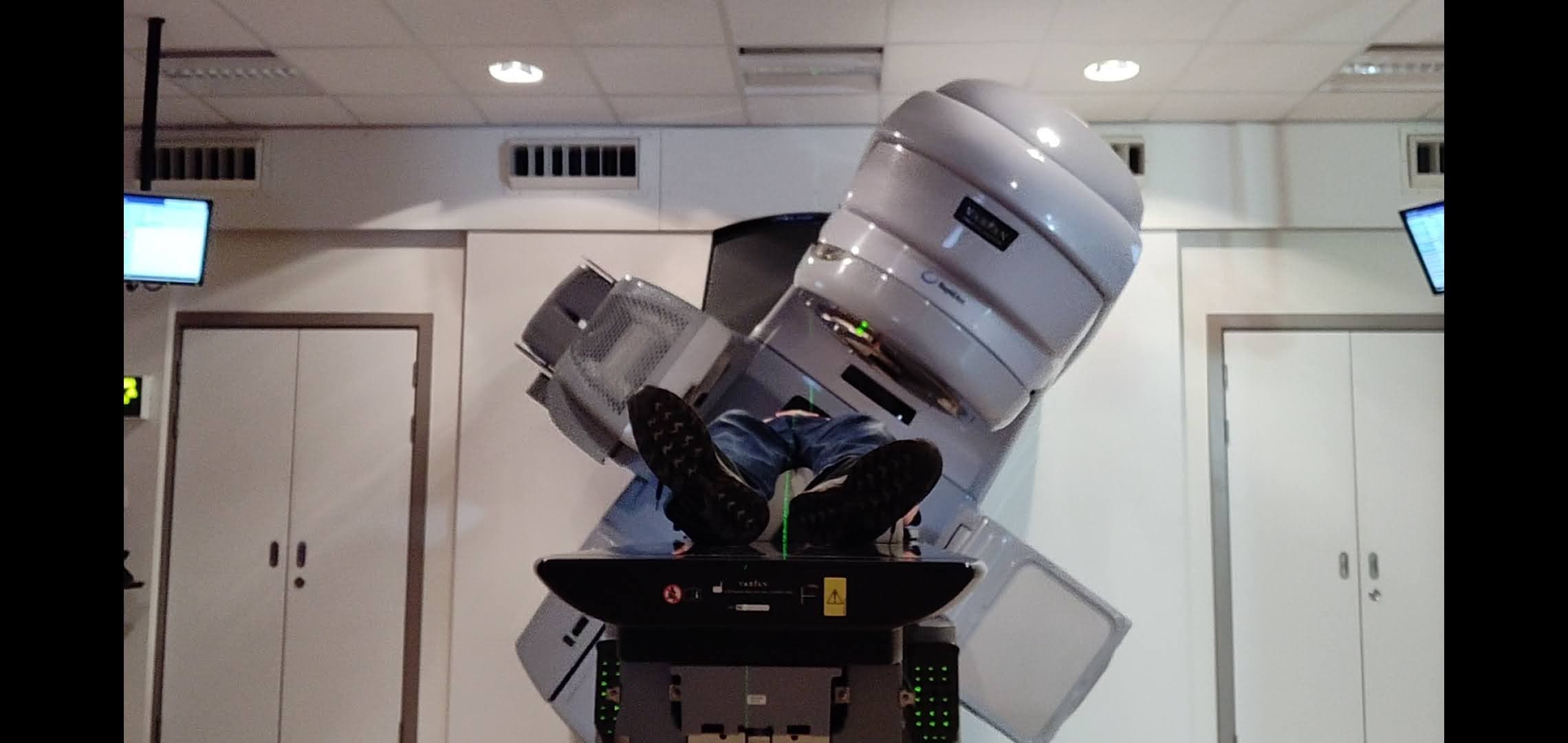
Once the machine passed over me for the final time I remember clenching both my fists and saying a little “yes!” to myself, 6.5 weeks and 33 sessions over! And the final time I’d need to put on the uncomfortable mask! You get the option at the end about if you want to keep the mask and take it home. I decided I wanted to keep it. I’m not sure why. Maybe I can pass it onto my kids and grandkids in the future? Maybe it will become a family heirloom that they can one day take onto the Antiques Roadshow! But for now it sits up in the loft so as not to scare the hell out of them!
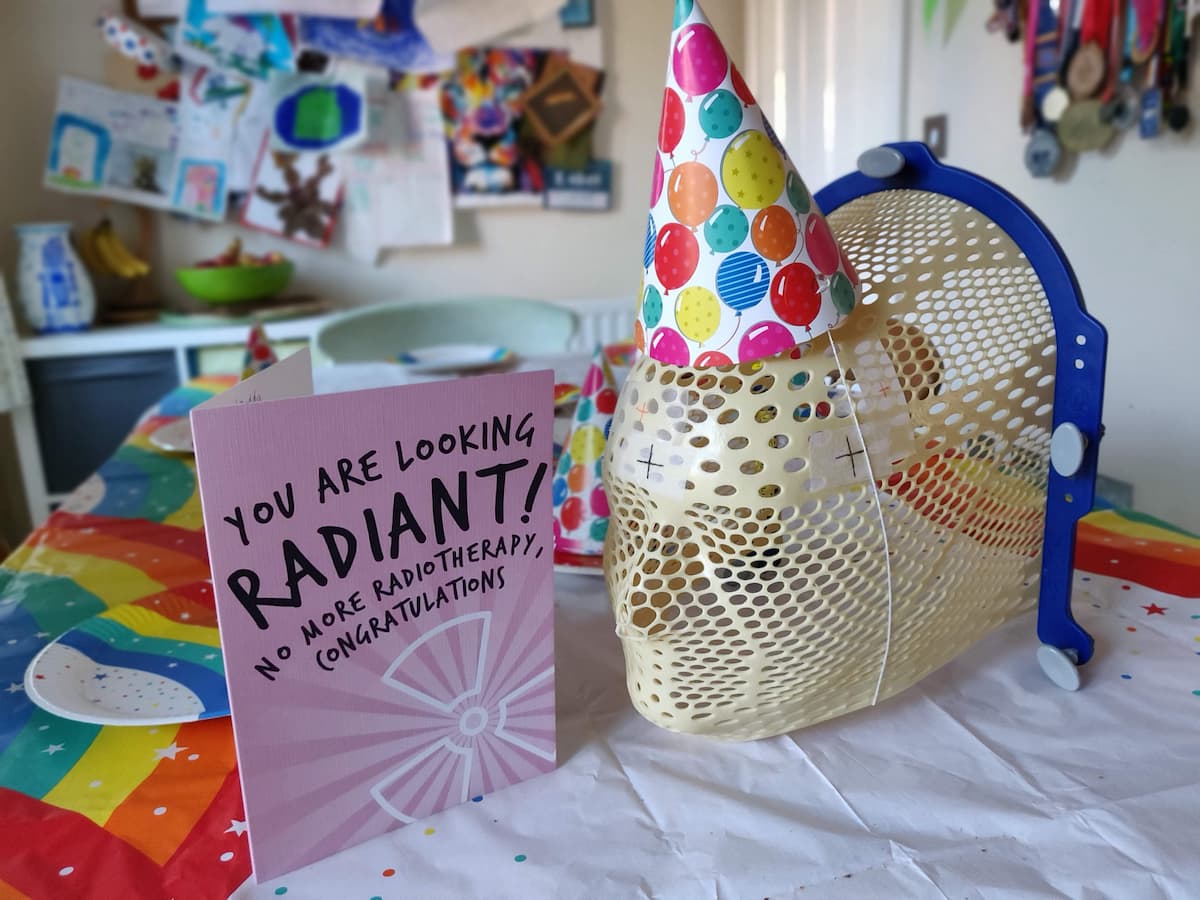
We had a little celebration as a family, a mini post-radiotherapy party with party plates, hats and balloons too! No jelly and ice cream though. Probably a good idea as I’m trying to cut down on sugar!
What’s next? - Friday 3rd December
After 6.5 weeks of going to the hospital everyday, Friday was unusual. I didn’t need to be anywhere or subject my head to both an internal and external suntan! I think I spent most the day sleeping trying to recover from the cumulative effects of the radiotherapy then had a takeaway (Indian) in the evening. All in all the treatment had been long and repetitive, but the side effects I had were all manageable.
The one thing I would say about the whole experience is it’s quite lonely. That’s not to say I’m not surrounded by friends,family and colleagues (past and present) but at the end of the day it’s me who is waiting around and then me lying in the machine(s) for the treatment and you can only ever do that alone. It certainly doesn’t help at the moment that Covid restrictions don’t allow anyone to be with you in the hospital. So if you are waiting 1.5 hours for a delayed machine. You are waiting alone.
But I’d like to say a huge thank you to all my friends / family and the wonderful NHS Transport service for getting me too and from each of my sessions over the 6.5 weeks.
So what next? Well I have approximately 6 weeks off over Christmas then should start 4-6 cycles of PCV chemotherapy some time mid-January. All being well this will last approximately 7 months. Well that’s a lot of 2022 planned for then! I’m hoping that around March they will be able to do another MRI scan of my brain and tell me what difference the radiotherapy made to Gary’s leftovers. Apparently it takes around 3 months for the brain to recover and repair after radiotherapy, and until it does they can’t see on the scans if it has made a difference.
So watch this space for more updates in 2022, where the remaining 5% of Gary is hopefully evicted from my head!
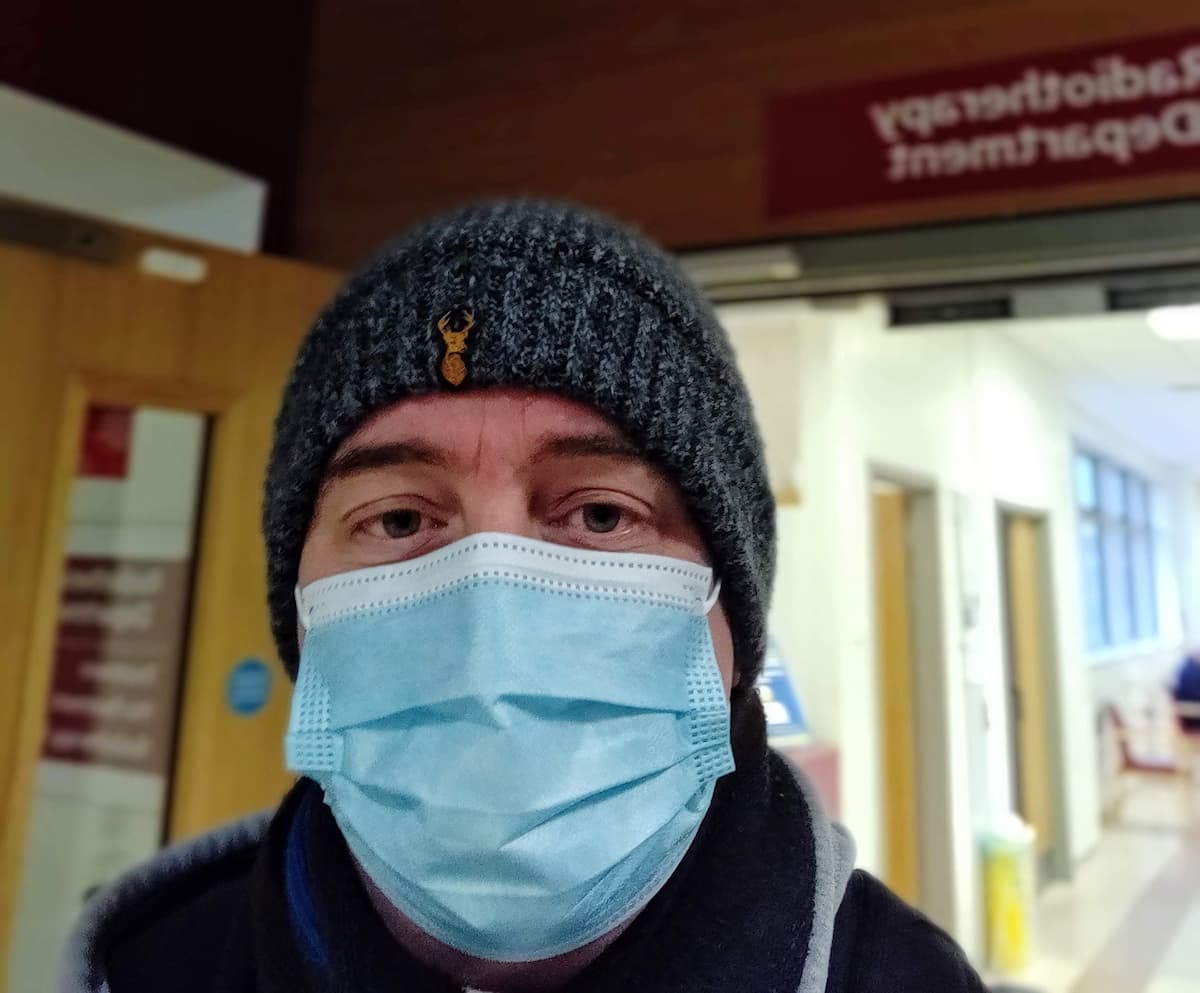
Oncology Meeting - Wednesday 29th December
So since my last update at the start of December, not much has really happened. I’ve had 5-6 weeks off, had a good Christmas with family and tried not to think too much about 2022 (although I must admit it’s almost impossible). As mentioned before, the plan moving forwards was radiotherapy, followed almost immediately by chemotherapy. At my initial follow-up meeting back in September very little was mentioned about the chemotherapy. This was intentional by the team, since getting my head around radiotherapy was enough for me at that point! So I’ve only had a few basic details about it all. This meeting was to tell me a lot more.
As with most of my meetings, it was a video call, it included two oncologists and a senior nurse. They went through a few of the details about the type of chemo I’m going to be having (it is called PCV), PCV stands for:
- P – Procarbazine
- C – Lomustine (CCNU)
- V – Vincristine
These are the three types of drugs I’m going to be taking for the next few months. Vincristine is taken intravenously, the other two drugs are prescribed to me and taken in pill form at home.
I’m going to be taking these drugs in what are called cycles. Each cycle is 42 days long, and I will have up to 6 cycles (assuming my body allows for it). A cycle consists of:
- Day 1 - Go to the hospital and sit while they give me Vincristine via a drip.
- Day 1 to 10 - take the Lomustine and Procarbazine every day at the same time each day
- Day 11 to 42 - This is a rest period for my body to recover from the chemotherapy drugs.
- Repeat this process up to 6 times if my body allows for it.
Now, the difference between the radiotherapy and chemotherapy is that radio is very targeted (hence my ‘sunburnt’ head!). But chemotherapy isn’t targeted at all, it is given to me and can have an impact on all the cells in my body. If you take a look at the potential side effects this is the reason why there can be so many!
A big negative of chemotherapy is it can have quite a big impact on my immune system. It reduces the white blood cell count in my body. These cells are used to combat infections. So the less white blood cells you have, the more susceptible to other illness’. This is what I mean when I mention “if my body allows for it”. At the start of each cycle, the hospital looks at my white blood cell count to determine if I am healthy and able to continue with the next cycle. If not then they may lower the drug dosages or if it’s terrible, pause the chemotherapy completely. Each and every person’s body reacts differently to the drugs, so I won’t know until I’m into the first couple of cycles as to how my body reacts. So it’s another journey into the unknown!
Six cycles at 42 days each, so I’m looking at around 7 months of chemotherapy! That’s quite a long time to try and not get sick! Especially during a global pandemic! Speaking of which, I asked about Covid and If I do end up catching it the NHS are able to give me special drugs to help my body combat the virus.
So it’s people in my position across the world who are in danger when a huge portion of a population refuse to take the vaccine. As if life isn’t bad enough when you have cancer, only to find going out people around you could make you even sicker! So yes, for the next 7 months I’m generally going to be avoiding people I don’t know, and asking friends and family I see to take a test before meeting with them. Not a great position to be in! I’ll get off my soapbox now…
The only disappointing part of the meeting was they were unable to give me specific dates for my treatment or the hospital it would be at. This isn’t the fault of the doctors, it’s just a scheduling and administration bottleneck given the pressure the NHS is under at the moment. They said I’d be receiving a few phone calls in the coming days to confirm dates etc. Until then, we wait!
Houston, we have dates! - Thursday 30th December 2021
Well, thankfully I didn’t need to wait long for the dates. I received a few phone calls the day after the meeting:
- Monday 10th January - chemotherapy pre-admission
- Tuesday 11th January - start of cycle 1
In the previous meeting, they also mentioned that I’d need to have another MRI scan to see what effect the radio has had on the remaining 5% of Gary, but they said this could take a while to schedule, and I may have started chemo before it actually happens.
Death to 2021 - January 1st 2022
As I said at the start of this very long blog post. Just when I thought 2020 was bad, 2021 comes along and proves me wrong! It has undoubtedly been one of the worst years of my life, but that being said I’ve achieved a lot (well up until August anyway!). I worked up until 2 weeks before surgery, so I managed to pack quite a bit into the first 8 months. My year in review:
- January: Spoke at FOSDEM21
- February: Spoke at London Web Performance
- March: Cloudflare Worker experimentation blog posts
- April: Diagnosed with a Grade 3 Brain tumour
- May: Spoke at Web Directions Lazy Load
- June: Lots of Hospital appointments
- July: Missed the F1 at Silverstone due to the Covid risk before my surgery date.
- August: Stopped work before surgery
- September: Had awake open-head brain surgery
- October: Recovery + Radiotherapy
- November: Lots of radiotherapy
- December: Turned 40 and got a Puppy
Not bad, all things considered! Here’s hoping for a better 2022! Fingers crossed the final 5% of Gary gets evicted from my head!
MRI Scan scheduled - Thursday 6th January 2022
So much for it taking a while to schedule the MRI! I received a phone call asking me to come in to hospital the next day (Friday) for my MRI scan. Not much notice, but the good thing (I hope) about this date is they should have the scans back for my pre-admission meeting, so you never know they may actually be able to give me an update on how the rest of Gary the prick is looking!
MRI Scan - Friday 7th January
You’d have thought by now that the thought of lying still in a tube doesn’t phase me, but it still does. There’s nothing particularly scary about it. It’s very loud and a little uncomfortable (and very boring). But other than the cannula for the contrast they inject, it’s not that unpleasant. Even so, I still get a little nervous before it happens. I think it’s because when you are in the machine alone with your thoughts, there’s no way to ignore the fact that you have cancer. It isn’t a bad dream that you are going to suddenly wake up from. It’s actually that you are lying in this machine (again) for 25 minutes!
Anyway, the scan was uneventful. Just another hurdle to jump over in the whole process!
Chemotherapy pre-admission - Monday 10th January
The meeting was a bit of a disappointment. I was expecting there to be a bigger team to discuss what was going to be happening, but in the end it was “only a nurse” (her words, not mine!). I managed to get a few questions answered, but I have many more for the consultants / doctors.
Unfortunately, due to it being a specialist cancer centre, Claire was unable to be at the meeting with me. She had to sit in the car and listen in while I had her on speakerphone. This is due to the current Omicron covid variant restrictions. The team mentioned that if I’d started just 2 weeks earlier, it wouldn’t have been an issue. But they’ve had quite a few patients partners walk into the centre who knowingly (or unknowingly) were covid positive, which obviously puts all patients at risk. So now they only allow patients in for meetings and treatment. And as a patient, you have to bring a negative lateral flow test from that day with you before you are allowed to be admitted into the centre.
On a more positive note, I’ve got all the dates for my cycles. So if all goes to plan, and I manage all 6, my ‘last day’ will be on the 20th September. Although I have no idea how long chemotherapy drugs stay in your system, so they may linger for a little while after that??
Chemotherapy cycle 1 start - Tuesday 11th January
I was incredibly nervous about the chemotherapy, I’m not 100% sure why, as the doctors had mentioned that it would likely not be as bad as the radiotherapy in my instance. I think it’s probably due to the longevity of the treatment. The surgery was scary but in all honesty if something went wrong I doubt I’d have known very much about it, I think it would have all just ended. Radiotherapy was localised long and repetitive, but once in the room it only took 5 minutes for the treatment, then you were done for the day. But with chemotherapy, I’d be taking the treatment “home with me”. With a tonne of possible side effects, and a total of up to 6 cycles lasting up to 7 months, I’m actually going to feel the effects of this for a long time into 2022. There’s pretty much no avoiding getting ill in some way once started.
Thankfully, the journey to the cancer centre is nowhere near as tedious as the hospital trips for radiotherapy, and I only need to go once every 42 days, the rest of the cycle is at home. Once I’d chosen a chair to sit in, the nurse came over and checked I was who I said I was, then explained what was going to happen (since it was my first cycle).
I was given the vincristine intravenously into my arm, then while that was happening I’d speak to the pharmacy team about the rest of my drugs. Unfortunately, the drip has to go into the back of the hand or wrist for this type of drug. This is because vincristine can cause damage to skin when outside of veins. The inside of my elbow (where’d I’d prefer it to be given) has a void behind the vein, so if there were a leak then the nurses wouldn’t know about it! Not ideal, but I can see why it is done! So in the end we managed to come to a compromise where I was cannulated on the side of my wrist behind my thumb.
Once the cannula was in my wrist, the drip only took 5 minutes to give me all the medicine it needed to. In this time, I spoke to the pharmacy team with Claire on the speakerphone, so she could listen in (she was sitting in the car due to covid restrictions). It was only then that I realised the sheer number of pills I was going to have to take at the start of each cycle. A minimum of 69 tablets over the first 10 days at different times of day, on top of the seizure tablets I already take! I’m very glad I don’t have problems taking tablets!
Once the drip had finished, that was it. I was sent home with a small green bag full of all the medication I’d need for the next 41 days. Before the process starts all over again!
Side effects It’s been just under a week into my first cycle as I’m writing this, and I have a pretty good idea as to how my body is reacting to it all. The first two days were pretty awful, very tired and lethargic and just generally not feeling 100%.
But It was into the third day that I started to feel the main side effect I’ve noticed. Eating my breakfast on the third day, the milk tasted metallic and my tongue / mouth were extremely sore. I’d love to say that this has improved, but it has actually got worse over the past days. Nothing I eat or drink tastes the same, and it has put me totally off food. It feels like I have a mouth full of ulcers. Not pleasant! Apparently this is a side effect of the vincristine so should hopefully diminish over time.
The only thing that has alleviated the pain is taking regular dosages of painkillers (more pills!), Corsodyl mouthwash, and Difflam mouthwash.
If anyone is in the same position, here’s a list of the foods I’ve had so far that still taste like anything palatable:
- Rice Pudding
- Custard
- Baked Beans
- French fries (no salt)
- Steak pie
- Boiled (or mashed) potatoes
- Sausages
- Gravy
I’ll keep this list updated as I find more foods that taste okay, I hope there are more, else I’m in for a very boring 7 months of food!
On a positive note, I haven’t experienced any nausea, which is what I thought may happen. But then again, I am taking 3 types of anti-sickness tablets! So maybe they are doing their job at the moment and I have that to look forward to later in the cycle? I hope not!
1p/19q Codeleted gene update
I mentioned 1p/19q Codeleted gene) before which will effect how effective the chemotherapy is against Gary, Thankfully it turns out that I do have this gene mutation, this is a good thing as it should mean that the chemotherapy should be more effective in my case! Yay for genetics!
Oncology Update - Wednesday 19th January
I was told this meeting was to discuss the results of my MRI scan, so I was quite nervous in the days leading up to it. But in the end it turned out to mainly be a catchup about how cycle 1 was going. I updated the team on the side effects I was experiencing and asked them a number of questions, one of these was how my brain was looking on the scan. Due to the fact that my brain is still healing from Decembers radiotherapy, they couldn’t tell me too much. But they did say that the tumour was looking “stable”, which I guess is good! They said that my next scan (date unknown) should tell us a lot more, as it will be past the 10-12 week cut-off for my brain healing from radiotherapy.
Chemotherapy cycle 1 end - Friday 21st January
So technically this isn’t the end of the cycle, but it is the end of taking all the chemo drugs for cycle 1! 10 days and 70+ tablets later, It’s been a busy week, and I’ve learnt a lot that I can take into the next 5 cycles.
So what have I learned in cycle 1?
Well, first thing is to make sure you are taking the correct anti-sickness pills! I’d mistakenly been taking the wrong ones for the first few days. When you are feeling like crap and half-asleep at 6 in the morning, this was an easy mistake to make! They both look the same in colour and shape and come with some wonderful side effects! So yes, I won’t be making that mistake again!
Another thing is to start using both sets of mouthwash and dosing up on constant painkillers from day 1. The mistake I made was to wait for the side effects to become almost unbearable, before contacting the cancer triage number. Hitting it hard from day 1 will hopefully make the first 4-5 days (the worst ones), more manageable!
I’ve also learnt that only 1 in 10 people on PCV chemotherapy get the jaw / mouth side effects like I have! I mean, I wouldn’t expect it any other way given the rarity of the type of tumour I have, where’s the fun in that, huh, body? What a stupid bag of meat.
Lastly and probably most important is the types of foods I can and can’t eat. After day 2 normal breakfast is out the window and replaced with food with an actual taste. By Day 5 my mouth starts to feel slightly better, at day 12 I was almost back to normal.
Now of course this is assuming the other 5 cycles are exactly the same as the first, but the Oncology team did say there would likely be a slight cumulative effect as the cycles progress, so prepare myself for it to get worse over time!
All in all, though, given the number of possible side effects, I feel I’ve got off lightly for my first cycle. I’m just hoping it stays that way for the following 5! But that’s totally out of my control. Here’s hoping my white blood count stays high enough to continue, and I don’t catch any illness’ over the next 8 months! This may be a big ask given I’m currently starting a phased return to work!
Ongoing work - Months of March / April 2022
Now, considering I’ve only been working a limited number of hours during my “phased return to work” period, I’ve felt It’s been very productive. Obviously not 100%, but I set myself a daily set of tasks I’d like to complete, then anything that doesn’t get done gets “bumped” onto the next day or later in the week. Obvious really when you think about it, but I’m really having to be that strict with myself, else I know I’ll end up doing full days again and burning myself out! Not good for me (or work either!). I’ve been logging all my working hours and what I’ve been doing to see what pattern emerged over my “recovery periods”. Interestingly, you can see a pattern. As time passes and the drugs work out of my system, I’m able to work slightly longer and achieve more each day. Some highlights at work for the past months include:
- Recruitment: The community and I are very much recruiting FE developers. I’ve been involved in all stages of this (CV sift, phone interview and face-to-face interviews).
- Joiners: We’ve had a number of new joiners in the community. So I’ve been involved in welcoming them to the department and making sure our guidance around the communities new starter “buddy system” is set out and well-documented.
But the absolute highlight for me has to be the GOV.UK team has managed to remove jQuery from all Frontend apps across GOV.UK.
Sorry to go into “work mode”, but this basically means 32 KB of compressed JavaScript has been removed that our users no longer need to download when they visit all GOV.UK pages. Now I know what you may be thinking, 32 KB that’s nothing! So that’s true for a single user, but GOV.UK see’s millions of users every month, so it multiplies to a huge data saving for all our users! I tweeted about the results we saw in our performance monitoring (RUM, Synthetic) and the response was quite crazy!
The performance data speaks for itself, really. I highlighted the fact that this has improved the web performance of GOV.UK for the users who really need it (our P95 users), These are users on limited data plans and low-spec devices. By improving performance for these users actually improves performance for everyone!
So a massive pat on the back to the GOV.UK team for getting this change out the door it’s been a slog but if you don’t remove tech-debt it will eventually drown you and stop you from moving forwards.
We also had some sad news in the community, Alex J a fantastic Lead Frontend Developer and great friend and colleague decided to leave the department to return home to Romania. I can’t tell you how genuinely gutted I was when I heard the news he was leaving, his dedication and knowledge on GOV.UK and his leadership in the Frontend community will be surely missed! I wish Alex all the best and hope our paths cross again in the future!
Sorry for that digression into work. I’m also happy that I’ve proved that I’m still able to work sans-Gary (the prick!). So now back to the “fun part”, my cancer treatment (what an odd statement!)
Oncology Update - Wednesday 6th April (morning)
As always, a busy start to the next cycle. Oncology review in the morning, chemotherapy treatment in the afternoon.
I was genuinely nervous about this meeting, as 2 weeks before I’d had yet another MRI scan. This was the first scan that would be able to “show anything”. Since it takes 3 months for the brain to “repair” after radiotherapy. In the last MRI scan, nothing could be said for certain, as damaged brain matter looks the same as a brain tumour on an MRI scan (talk about ironic!).
But anyway, the meeting went really well. My bloods looked great, and the scan was described as “stable” or in other words what is left of Gary hadn’t grown. The Oncologist at one point also said that the tumour was very difficult to see! I think that’s the best news I could have had! It certainly makes up for the nights leading up to the meeting where I would wake up thinking about it!
The chemotherapy would be going ahead as planned on the same dosage of Vincristine I’d had before.
Chemotherapy cycle 3 start - Wednesday 6th April (afternoon)
Nothing really to report here, only we turned up an hour early for my appointment! I think my frazzled brain got the time wrong, thankfully the cancer centre were able to fit me in any way. I had the infusion, but then had to wait awhile for my other medication (it takes time to prepare). I think my punctuality caused that issue, not the nursing team!
But once completed, I set off on my merry way with a body full of vincristine and a bag of 90+ tablets.
Chemotherapy cycle 3 end and recovery - Saturday 16th April
As I’ve found with the previous cycles, it starts off slowly in the first few days, then ramps up around day 3 or 4. This is while the body adjusts to the concoction of drugs sent in to kill cells (mainly the bad ones, but there is friendly fire with chemotherapy as it isn’t targetted like radiotherapy).
I was able to work a couple of hours on the Thursday, which got me thinking “oh, maybe this cycle won’t be so bad”. Boy was I wrong about that! I think I jinxed it, so I won’t be making that mistake again in the future!
I won’t go into a day-by-day account, but let’s just say the cycle turned out to be worse than cycle 1. I’ve never felt so bad for so many days with no end in sight! The fact that I knew I needed to keep taking tablets every day that were only going to make me feel even worse, is a horrible feeling. It’s a real struggle to make yourself take them at some points in the 10-days! Some wonderful side effects from this cycle (in no particular order) have been:
- Nausea (no vomiting, thankfully)
- Weakness (as in, can’t get out of bed or even move)
- Headaches (thank you paracetamol!)
- Light-headed and dizziness (even when sitting on the sofa)
- Spiked blood pressure
- Lack of appetite
- Random pains all over my body
- Insomnia
And to top it all off, I now seem to have developed Tinnitus in both ears, this is a known side effect of the vincristine and can be temporary or permanent (only time will tell).
So, yes, if you are reading this and are new to chemotherapy it probably isn’t a fun read, but as they say “no pain, no gain” (FYI: don’t say this to a person going through chemo unless you want a stern look or a strongly-worded letter!).
So what have I learned in cycle 3?
- Don’t go into any new cycle expecting the same side effects from the previous cycles, you are setting yourself for a fall!
- Only take the anti-sickness pills if you are actually feeling sick (see my comments below on this)
- Make sure you are open and honest with the team managing your treatment, keep them updated regularly! They are there to help you!
- Try to focus on the recovery period, it takes a while for the drugs to leave your system. It can take up to 6 weeks for some people (it’s likely you won’t feel “normal” again until this happens).
Just to jump back to point 2, there’s conflicting information here. You are told to take them only when you feel sick, but also that it is easier to cure the “feeling of sickness” than the sickness itself! So yes, get in a time machine and see if you are likely to feel sick or be sick, then choose the correct path!
The reason why this point is so important is that each drug you take has its own unique set of side effects for your body. I found the anti-sickness pills were making me extremely weak and tired, so I stopped taking them midway through the cycle. Only then to find that the last few days of the cycle I’d suffer from terrible Insomnia, because I no longer had the weakness and tiredness from the anti-sickness pills! It’s a minefield! I’ll be mentioning all this at my Oncology review meeting at the start of Cycle 4 (May 18th 2022), maybe they can adjust my drugs in some way?
To end on a more positive note, I’m now over half-way through! 3 cycles down, 3 to go! Roll on October, and at some point back to “normality”.
So as before I likely won’t be updating the post again until after my next cycle ends (end of May), unless something drastic happens!
Diagnosis Anniversary - Thursday 21st April
So here’s an anniversary that I never thought I’d be ‘celebrating’ in a million years, but here we are. Celebrating is totally the wrong word, but it is a significant date, as 1-year ago today it felt like the whole ground fell from under me. My life, what was once a path paved and walked day by day, suddenly became a fog of unknown obstacles and fear. So many questions that my whole family and I had no idea about! I mean, why would you read into brain cancer if you didn’t need to?!
It has been both the longest and shortest year of my life, when you live it day-to-day everything drags! Radiotherapy is relentless, a 6-week-long tidal wave that never seems to end. Avoiding everyone during chemotherapy is depressing because you are scared to even catch a common-cold! It’s been a real rollercoaster of emotions!
Some particular points that stand out to me:
Scariest moments
- Seeing the size of Gary for the first time over the video call with the surgeon!
- Closely followed by heading (hah!) into the surgery for my awake craniotomy, Not knowing if I was going to wake up parallelised, partially-parallelised, or even wake up at all!
Low points
- Obviously being diagnosed with brain cancer is up there at the top of the list, but also telling my wife, and parents and sister of the diagnosis.
- The week between initial diagnosis and actually having more detailed information from the hospital (that was a long week!)
- Seeing the look on my mom’s face when we were initially shown the size of Gary.
- Having those horrible conversations with my wife about what to do if the “worst should happen”
- This list could go on for a while, so I’ll spare you and stop at 4!
High points
- Realising there were lots of options available, and I shouldn’t see this as a “death sentence”.
- Seeing the outpouring of support both personally (family & friends), at work, and across the whole web community when I first announced my diagnosis.
- Being told they’d been able to remove 95% of the tumour with little to no-damage to any of the good parts of my brain.
- Finishing radiotherapy after a lot off back-and-forth to the hospital every week day for 6 weeks!
- Receiving the UCS Lego Millennium Falcon from some very kind friends in the Web Performance community (build in progress at the moment!)
- Realising I can still think (and work) in the post-Gary world (“full recovery” may take a while, but I can do it!)
- My wife raising over £2,700 for The brain Tumour Charity for her entry into the 2022 London Marathon. Thanks to everyone who donated, you rock!
- Seeing how we have come together as a family to cope with the scary and ever-changing world of the cancer diagnosis and treatment process.
To jump on the last point a more. I can’t thank my close family and friends enough over what has been an incredibly tough year! I certainly couldn’t have made it this far without the daily support of my wife, kids, parents, sister and her husband, and my mother-in-law.
Admittedly, my kids are the absolute perfect age to drive me to distraction, but that’s exactly what is needed. Life would be so boring without their daily arguments and tantrums!
And last (but certainly not least!), a huge thank you to the help, support and dedication of the whole of the NHS workers I’ve interacted with over the past year (so so many individuals!). Without them and modern medicine, I hate to think where I would be now, 1-year into my diagnosis!
Treatment Tally Table
I thought I’d pull together a tally of all the treatment I’ve had along the way in my quest to evict Gary from my skull, which I will keep updated below.
As I’ve said before, thank you again to the NHS. All this would have cost a fortune in certain countries without universal healthcare (sorry American readers)!
| Treatment | Number | Finished? |
|---|---|---|
| Radiotherapy | 33 | Yes |
| Chemotherapy Cycles | 3 | No |
| MRI Scans | 5 | No |
| CT Scans | 3 | No |
| PET Scans | 1 | Yes |
| Major Surgery | 1 | Yes? |
Post changelog:
- 21/04/21: Tumor first diagnosed.
- 12/05/21: Initial post published.
- 15/05/21: Posted 3 new updates from the week. Next appointment on the 20th May.
- 19/05/21: Added information about another seizure.
- 21/05/21: Added information about the pre-operative assessment appointment.
- 25/05/21: Added update about the weekend and another seizure I’ve had.
- 29/05/21: Added information about obtaining my scan data and a different type of seizure.
- 03/06/21: Added update on date for memory test and overall symptoms.
- 07/06/21: Added steroid and reduced seizures update.
- 10/06/21: Added update from latest Neurologist meeting.
- 11/06/21: Update on first ‘core feature’ seizure I’ve had in 2 weeks.
- 19/06/21: Added an update about the sleepy seizure and an epiphany.
- 18/07/21: Added an updates about the month of July and “Between Life and Death”.
- 23/07/21: Update on the latest timings and the surgery info I’ve been given.
- 26/07/21: Pre-surgery MRI scan update.
- 01/08/21: Scan results and swelling symptoms update.
- 06/08/21: Back on the ‘roids and finally a productive day!
- 12/08/21: The highs and lows of steroids and finally some information on an operation date!
- 23/08/21: Added info about a surgery date and the fact I had another seizure.
- 27/08/21: Surgery cancelled, and an update on the very long week.
- 04/09/21: New surgery date is looking promising update, fingers crossed it will be next week!
- 08/09/21: Added update on the scans today and my final post for a little while.
- 21/12/21: Added a huge post-surgey update on the recover, radiotherapy and future plans.
- 17/01/22: Added an update about my chemo meetings and first cycle. Also added a tally table for all the treatment I have recieved so far.
- 17/01/22: Added an update to my 1p/19q Codeleted gene result, thanks to Miles Mandelson for reminding me about this result.
- 24/01/22: Added update on Cycle 1 and 2 of chemo and the oncology meetings
- 19/04/22: Added update on Cycle 3 recovery and return to work.
- 21/04/22: Added update on the 1 year diagnosis anniversary.
